Today I found a rather nice article that shows that scientists can now grow bones from using plastics. I will copy and past the entire article here.
Neo-organs: Scientists use plastics to help the body make new bone
January 15, 2001
Web posted at: 11:21 AM EST (1621 GMT)
(CNN) — Physicians tell us the human body is a marvel of engineering. It can adapt to survive in many different environments, it can build muscle to grow stronger and can even heal itself. Its major flaw is it doesn’t come with spare parts. But scientists are working on ways to address that — at least for one body part. They’re developing exciting new strategies to make new bone.By David Terraso
CNN.com Associate Editor
Imagine a day when you show up to the emergency room with a broken leg. Instead of putting your leg in a cast for an entire month or two, doctors inject the fractured site with a plastic liquid that hardens in about a week, providing enough support for you to walk on it.
But this scaffolding provides more than structural support, it actually helps your bone heal. Built into the plastic scaffold are proteins called growth factors, which are released as the plastic degrades inside your body. The proteins help entice blood vessels from the healthy surrounding bone to invade the damaged area, bringing nutrients that the new tissue needs to survive. After a while, all the plastic has safely disintegrated, leaving you with new bone where the fracture once was.
While healing a broken leg is certainly important, this technique, if perfected, could also be used to replace bone destroyed by cancer, or in a spine fusion to treat a ruptured disk. By fusing two vertebrae together, the surgeon can eliminate the pain.
Current strategies
Each year an estimated 300,000-600,000 patients have bone fractures that require doctors to augment the body’s natural healing process. Additionally, many patients have conditions in which large segments of bone are destroyed or must be removed.
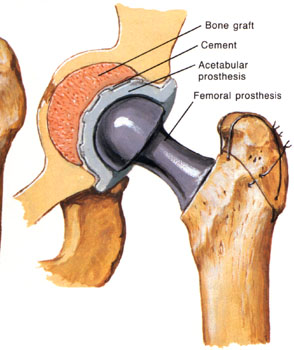
Currently, if a patient needs new bone, the best way for the doctor to obtain it is to perform an autograft — to scrape the bone from another site on the patient’s body, usually the hip. Taking the bone from the patient’s own body does two things. It eliminates the possibility that the tissue will be rejected by the immune system, and the growth factor proteins and stem cells in the scraped bone help it grow into new bone as well as induce the surrounding healthy bone to grow into it.
While this technique works, it’s akin to robbing Peter to pay Paul, leaving the patient with a damaged hip. Since the scraped bone is in tiny pieces, it provides no structural support. And there’s only so much bone that can be harvested, so if a patient needs more than his hip will give him, doctors often resort to a second technique known as allografting — taking the bone from a deceased donor.
Allografting has its own problems. Because the tissue is dead, it has none of the growth inducing properties the living bone has. But it provides more structural support, because doctors use an entire section of bone from the donor, rather than just bone scrapings.
From plastics to people
The challenge facing researchers is to find a material that has the structural support of the allografts, while having the growth-inducing properties of the self-harvested autografts. The ideal material would also be able to degrade safely inside the body, leaving only newly formed bone behind.
Dr. Antonios Mikos, a chemist at Rice University in Houston, Texas, and vice president of the Tissue Engineering Society, thinks he and other researchers have found that material: plastics.
“The biggest problem in engineering organs is getting the blood supply to them,” said Mikos. Plastics may offer a way to solve that problem.
Even if the doctor can get new bone to form, unless blood can get to the new tissue, it will die, leaving the patient no better off than before the operation. So the trick is to encourage cells and blood vessels that are already in the surrounding area to grow into the new bone. Loading plastics to release proteins known as growth factors could do just that.
|
| Mesenchymal stem cells (shown in white) are attached to a biodegradable plastic scaffold. The stem cells, which are taken from bone marrow, can grow into bone, cartilage or other structural tissues depending on the environment they are in. |
|
The main advantage of using plastics is that they can be injected, eliminating the need to cut open the patient. Their weight-bearing capacity can also be adjusted, depending on their chemical make-up, to be as strong as a thighbone, or lighter and more porous, such as a jawbone.
Another big advantage of plastics, said Mikos, is that scientists can control the rate at which they degrade. Tuning these plastics to degrade at the same rate as the new bone is formed is extremely important. If they disintegrate too quickly, they lose structural support — if they don’t disappear fast enough, new bone will have trouble forming. To make matters even more difficult, the plastic will have to degrade at a different rate depending on which bone it is in and how much weight the bone has to carry, Mikos explained.
Researchers have already been using certain plastics, which already have FDA approval for specific uses inside the body. But since no single material can work for every bone, Mikos is trying to develop new kinds of plastics that will be specifically designed to work as, say, a thighbone, or a vertebra, being able to handle the proper load and degrade at the correct rate for each bone. It’s a difficult task, he admitted, but one that has great promise.
In addition to inducing surrounding cells to make bone, another strategy researchers are pursuing is seeding the plastic scaffolds with stem cells. Taken from bone marrow, stem cells have the ability to turn into many different kinds of cells depending on the environment they are in. The stem cells on the scaffold would turn into bone themselves. For patients who don’t have enough bone-growing cells in the surrounding area, such as the elderly, smokers, or patients who’ve undergone radiation therapy, seeding the scaffolds with stem cells will allow bone to grow where it otherwise would not have been able to.
“The main obstacle to the stem cell approach is in large defects, larger than half a millimeter. The cells on the interior of the scaffold tend to die because they can’t get enough nutrients from adjacent blood vessels,” said Mikos.
One solution may be to seed the plastic scaffold with both the growth factors and stem cells, but for patients such as those mentioned above, the growth factors wouldn’t work very well. It’s also unclear how much growth factor is needed in humans. The initial animal research showed the growth factor proteins work well, but as scientists test this method on species that are closer in makeup to humans, they find they have to use a lot more of these proteins, which may not be safe in these high doses. Fortunately, there is some promising research that hopes to get around this problem.
The natural solution
“Scientists have long known that exercise helps maintain and strengthen bone,” said Dr. Robert Guldberg, a biomechanical engineer at the Georgia Tech/Emory Center for the Engineering of Living Tissues.
Creating mechanical stress on the bone can help stimulate bone to repair itself. Using this idea, Guldberg is working on using a hydraulically activated implant inside the injured area to accelerate healing by putting stress on the bone defects.
“During normal function, bone is a load-bearing tissue and strategies for engineering bone regeneration must therefore consider the mechanical loading environment in the body,” Guldberg explained.
He could also use this system to force the nutrients from the surrounding cells into the interior of the defect, allowing those cells to thrive.
In keeping with his philosophy of mimicking the natural healing process, Guldberg is also growing cartilage scaffolds in the lab and implanting them into bone defects. During normal fracture healing and growth, cartilage produces growth factor proteins among other things that entice surrounding cells to make new bone. The benefit of using cartilage over plastics may be that “since it’s the natural scaffold for bone anyway, there might be a natural tuning of the scaffold degradation process with new bone formation,” said Guldberg.
Custom-fitted parts
Growing bone inside a particular defect is one thing. In some patients there is still the problem of forcing the new bone to grow into a particular shape. For a patient with cancer of the mouth, part of the jawbone sometimes needs to be removed to prevent the cancer from spreading. Replacing the diseased bone with a new one that looks and operates just like a healthy jawbone is extremely important in helping the patient resume a normal life.
Dr. Michael Miller, deputy chairman of the Department of Plastic Surgery at M.D. Anderson Cancer Center in Houston, Texas, is working on using plastic molds to help grow new bone into specific shapes.
A big problem in dealing with patients who have cancer is that many of them have to undergo radiation therapy, which harms many of the bone-producing cells in the surrounding tissue, said Miller. So it’s particularly challenging to grow new bone in those areas.
To address this problem, Miller has been developing a new method based on filling plastic molds with ground up bone from autografts and placing them next to the patient’s hip. This technique accomplishes two things — the mold forces the bone to grow into a particular shape so it can be custom fitted into the defect, and since the bone is growing next to healthy tissue, it can use the undamaged cells to form blood vessels and new bone, potentially overcoming the radiation problem. So far, Miller has tested this technique in sheep with encouraging results.
Combining the fields of gene therapy and tissue engineering, some researchers are trying to induce the body to make more growth-inducing proteins. Dr. Scott Boden, a spine surgeon at Emory University who works with Guldberg, has discovered a gene that encodes for a bone-making protein called Lim Mineralization Protein. By genetically engineering cells to make more of this protein, scientists hope to encourage bone growth.
“One of the applications being tested is to relieve back pain by implanting these genetically engineered cells in between adjacent vertebrae, causing them to fuse with new bone formation,” said Guldberg.
Although there is still a lot of testing to be done before any of these techniques become part of everyday medical practice, researchers are optimistic they are on the right track.
“Since no single technique is going to work in all situations, pursuing several strategies increases our chances we’ll be able to treat the wide range of conditions that affect patients,” said Guldberg.
The day when we can grow our own spare parts may not be that far away.
While this technology can not be directly used to increase our height through just adding some of the plastic to the ends of our bones, it can be used in collaboration with others to create a height increase method. The article found from the boards is a rather old one, back from 2001. You can get to it by clicking HERE.
 I think this is an appropriate question to ask my regular readers. I know who you are out there. There really is only 3 of you, maybe 4 but I still wanted to ask and get some feedback from you guys. Some of you come and check this site like 10 times a day, which is cool by me. Any traffic and eyeballs who are interested in what I have to say and write is nice. If this turns into an obsession of yours, it might a good idea to take a break from this site. I do try to write 3-4 blog posts a day, sometimes even up to 7 articles, but sometimes I don’t have enough energy or motivation to do much.
I think this is an appropriate question to ask my regular readers. I know who you are out there. There really is only 3 of you, maybe 4 but I still wanted to ask and get some feedback from you guys. Some of you come and check this site like 10 times a day, which is cool by me. Any traffic and eyeballs who are interested in what I have to say and write is nice. If this turns into an obsession of yours, it might a good idea to take a break from this site. I do try to write 3-4 blog posts a day, sometimes even up to 7 articles, but sometimes I don’t have enough energy or motivation to do much.