Me: This post will be a far more detailed analysis on the growth plate and the surrounding bones.
Interestingly, the writer of the source link is Dr. Brighton who I have done research on his work. Source link HERE. This entire post is a repost of material that Dr. Brighton has written up for a Chapter on Growth Plate growth for a class probably at the University of Pennsylvania.
CHAPTER 2 : NORMAL BONE FORMATION
SECTION ONE: EPIPHYSEAL BONE FORMATION
CARL T. BRIGHTON
Organization of the Growth Plate
Blood Supply of the Growth Plate
Structure and Function of the Growth Plate
Cartilage Component
Matrix Component
Fibrous and Fibrocartilaginous Components
The vast majority of the longitudinal growth of a typical mammalian long bone occurs at the ends of the bone in platelike structures termed growth plates. Both growth plates, one at the proximal end and the other at the distal end, are peripheral extensions of the primary center of ossification, a structure that arises in the midportion of the cartilaginous anlage of the bone-to-be during early fetal life. Originally the primary center of ossification grows and expands centrifugally in all directions. However, as it continues to expand, endochondral bone growth soon becomes confined to the growth plates (Fig. 2-1).
As growth continues, the growth plates grow away from each other. In each end of each long bone, at a time characteristic for each species of animal, a secondary center of ossification, termed the epiphysis, appears. It likewise grows and expands centrifugally in all directions, although much more slowly than did the primary center. As the distance between the growth plate and the epiphysis gradually decreases, the portion of the epiphysis that faces the growth plate closes and becomes sealed with condensed bone, termed the terminal bone plate or simply the bone plate.(78) Thereafter the epiphysis assumes a somewhat flattened hemispheric appearance and slowly fills out the remaining end of the long bone.
From the above it should be apparent that there is no single acceptable term for the growth plate proper. “Epiphyseal growth plate” or simply “epiphyseal plate” is incorrect, for these terms confuse the growth plate with the epiphysis. Rubin(48) introduced the term “physis” or “physeal segment” in an attempt to avoid this confusion. Physis, from the Greek word phyo meaning to grow or growth, is not sufficiently descriptive when referring to such a discrete morphologic structure as the growth plate. “Physeal segment” is more descriptive than physis alone, but it is a poor blending of the Greek and the English. Therefore, in order to avoid confusion and to be grammatically correct, the term growth plate will be used in this chapter.
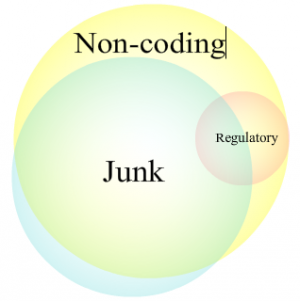
ORGANIZATION OF THE GROWTH PLATE
The typical, fully developed growth plate in the mammalian long bone consists of various tissues acting together as a unit to perform a specialized function and, as such, is an organ. The specialized function, of course, is longitudinal growth. Based on tissue content alone, the growth plate may be divided anatomically into three components: a cartilaginous component, itself divided into various histologic zones; a bony component, or metaphysis; and a fibrous component surrounding the periphery of the plate comprising the groove of Ranvier and the perichondrial ring of LaCroix. How the growth plate synchronizes chondrogenesis with osteogenesis or interstitial cartilage growth with appositional bone growth at the same that it is growing in width, bearing load, and responding to local and systemic forces and factors is a fascinating phenomenon the key features of which are only beginning to be understood at the present time. This chapter will discuss the structure and function of the growth plate in light of those processes that are known.
BLOOD SUPPLY OF THE GROWTH PLATE
Each of the three components of the growth plate has its own distinct blood supply (Fig. 2-2). (13,16,56) The epiphyseal artery supplies the epiphysis, or the secondary center of ossification, which itself is not part of the growth plate. Small branches arise at right angles to the main epiphyseal artery in the epiphysis and pass through small cartilage canals in the reserve zone to terminate at the top of the cell columns in the proliferative zone.(56) Each small branch from the epiphyseal artery arborizes in rakelike fashion to supply the top portion of from four to ten cell columns. The proliferative zone, therefore, is well supplied with blood. None of the branches from the epiphyseal arteries penetrate the cartilage portion of the growth plate beyond the uppermost part of the proliferative zone; that is, no vessels pass through the proliferative zone to supply the hypertrophic zone.
The metaphysis is richly supplied with blood both from terminal branches of the nutrient artery as well as from the metaphyseal arteries arising from the ascending cervical arteries. The nutrient artery supplies the central region of the metaphysis, perhaps as much as four fifths of the metaphysis, while the metaphyseal vessels supply only the peripheral regions of the metaphysis. Terminal branches from the nutrient and metaphyseal arteries pass vertically toward the bone-cartilage junction of the growth plate and end in vascular loops or capillary tufts just below the last intact transverse septa at the base of the cartilage portion of the plate. The vessels turn back at this level, and venous branches descend to drain into several veins that eventually terminate in the large central vein of the diaphysis.(37,41) All (14) or most(3) of the vascular loops are closed, and microhemorrhages from the vascular loops probably do not occur. No vessels penetrate the bone cartilage junction beyond the last intact transverse septa; that is, no vessels pass from the metaphysis into the hypertrophic zone.
The fibrous peripheral structures of the growth plate, the groove of Ranvier and the perichondrial ring of LaCroix, are richly supplied with blood from several perichondrial arteries.
 |
FIG. 2-1 Drawing depicting the two growth plates of a typical long bone toward the end of fetal life Each growth plate is a peripheral extension of the original primary center of ossification that arose in the middle portion of the cartilaginous anlage of the bone-to-be early in the fetal period. |
 |
FIG. 2-2 Drawing showing the blood supply of a typical fully developed growth plate. (Brighton CT Structure and function of the growth plate Clin Orthop 136:23 32, l978) |
While the metaphysis and the fibrous peripheral components of the growth plate have an abundant blood supply, only the proliferative zone of the cartilage portion of the growth plate is adequately supplied with blood. There are no vessels in the hypertrophic zone of the fully developed growth plate; hence, that zone is entirely avascular. This avascularity has important implications for chondrocyte metabolism and matrix calcification.
The blood supply of the human femoral capital growth plate has been studied thoroughly by Chung16 and, in general, is similar to that described above for a typical growth plate. Epiphyseal arteries arising from the ascending cervical branches of the medial and lateral femoral circumflex arteries were the sole supply of the epiphysis in 82% of the femoral heads studied by Chung. However, in 28% of the femoral heads, the epiphysis was also supplied by one or two branches of the artery of the ligamentum teres femoris (Fig. 2-3). The metaphysis is supplied with blood from terminal branches of the nutrient artery as well as from metaphyseal arteries arising from the ascending cervical arteries. The fibrocartilaginous peripheral structure of the femoral capital growth plate is richly supplied with blood from several perichondrial arteries arising from the ascending cervical arteries.
STRUCTURE AND FUNCTION OF THE GROWTH PLATE CARTILAGE COMPONENT
The cartilage portion of the growth plate begins at the top of the reserve zone and ends with the last intact transverse septa at the bottom of the cell columns in the hypertrophic zone. It has been divided into various zones according to morphology or function (Fig. 2-4). The reserve zone begins just beneath the secondary bony epiphysis, followed by the proliferating zone and the hypertrophic zone. The hypertrophic zone is sometimes further subdivided into the zone of maturation, the zone of degeneration, and the zone of provisional calcification.
 |
FIG. 2-3 Drawing showing the blood supply of the capital femoral growth plate. (RZ = reserve zone; PZ = proliferative zone; HZ = hypertrophic zone) |
RESERVE ZONE
The reserve zone lies immediately adjacent to the secondary bony epiphysis. Various terms have been applied to this zone, including resting zone, zone of small-size cartilage cells, and germinal zone. However, these cells are not resting, are not small in comparison with the cells in the proliferative zone, and they are not germinal cells. They appear to store lipid and other materials and perhaps are held in reserve for later nutritional requirements. If that is true, the term reserve zone may be appropriate. The cells in this zone are spherical, exist singly or in pairs, are relatively few when compared with the number of cells in other zones, and are separated from each other by more extracellular matrix than are cells in any other zone. The cells in the reserve zone are approximately the same size as the cells in the proliferative zone.(12) The cytoplasm exhibits a positive staining reaction for glycogen. Electron microscopy reveals these cells to contain abundant endoplasmic reticulum, a clear indication that they are actively synthesizing protein. They contain more lipid bodies and vacuoles than do cells in other zones(12) but contain less glucose-6-phosphate dehydrogenase, lactic dehydrogenase, malic dehydrogenase, and phosphoglucoisomerase. (29) The zone also contains the lowest amount of alkaline and acid phosphatase,(30) total and inorganic phosphate, calcium, chloride, potassium, and magnesium.(58) The matrix in the reserve zone contains less lipid,(24) glycosaminoglycan, protein polysaccharide, moisture, and ash(35) than the matrix in any other zone. It exhibits less incorporation of radiosulfur (35S) than any other zone and also shows less Iysozyme activity than the other zones.(51) It contains the highest content of hydroxyproline of any zone in the plate. (24) Collagen fibrils in the matrix exhibit random distribution and orientation. Matrix vesicles are also seen in the matrix, but they are fewer than in other zones. The matrix shows a positive histochemical reaction for the presence of a neutral mucopolysaccharide or an aggregated proteoglycan.
Measurements of oxygen tension in the extracellular space in the different zones of the growth plate reveal PO2 to be low (20 5 + 2.1 mm Hg) in the reserve zone.(7) This probably indicates that the blood vessels that pass through this zone in cartilage canals to arborize at the top of the proliferative zone do not actually supply the reserve zone itself.
The chondrocytes in the reserve zone either do not proliferate or do so only sporadically. Therefore, the zone is not a germinal layer containing the so-called mother cartilage cells. As a matter of fact, the function of the zone is not clear. The high lipid body and vacuole content may mean that these materials are being stored for later nutritional requirements. and in this sense, the function of the zone is one of storage.
 |
FIG. 2-4 Drawing depicting the various zones of the cartilaginous portion of the growth plate. (Brighton CT Structure and function of the growth plate. Clin Orthop 136:23 32, 1978) |
PROLIFERATIVE ZONE
The spherical, single or paired chondrocytes in the reserve zone give way to flattened chondrocytes in the proliferative zone. They are aligned in longitudinal columns with the long axis of the cells perpendicular to the long axis of the bone. The cytoplasm stains positively for glycogen. Electron microscopy shows the chondrocytes to be packed with endoplasmic reticulum.(12,20) Point-counting analysis reveals the percent of the cytoplasmic area occupied by endoplasmic reticulum to increase from 14.9% at the top of the zone to 40.1% at the bottom of the zone. (12) Biochemical analyses reveal the zone of proliferation to contain the highest content of hexosamine, (19, 24) inorganic pyrophosphate,(30) and sodium, chloride, and potassium.(53) The proliferating zone shows the highest incorporation of 35S of any zone in the growth plate, and it also has the highest level of Iysozyme activity.(5l)
Tritiated thymidine autoradiographic studies have indicated that the chondrocytes in the proliferative zone are, with few exceptions, the only cells in the cartilage portion of the growth plate that divide.(25)The top cell of each column is the true “mother” cartilage cell for each column, and it is the beginning or the top of the proliferating zone that is the true germinal layer of the growth plate. Longitudinal growth in the growth plate is equal to the rate of production of new chondrocytes at the top of the proliferating zone multiplied by the maximum size of the chondrocytes at the bottom of the hypertrophic zone.(53) Kember (25) showed that the average number of new chondrocytes produced daily in each column in the growth plate of the proximal tibia in the rat was five. Since the average diameter of the chondrocyte at the bottom of the hypertrophic zone is about 30 um, the rate of growth from that particular growth plate is about 150 um/day. He further calculated that each division of a top cell in a cell column contributes 29 cells.(26) This means that each division of a top cell eventually contributes 0.9 mm of longitudinal growth to the rat tibia (29 x 30 um = 870 um). Complete growth of the rat tibia would require 40 to 50 top-cell divisions. These principles (but not the absolute numbers) presumably hold true for all mammalian growth plates.
The matrix of the proliferating zone contains collagen fibrils, distributed at random, and matrix vesicles, confined mostly to the longitudinal septa. The matrix shows a positive histochemical reaction for a neutral mucopolysaccharide or an aggregated proteoglycan.
Oxygen tension is higher in the proliferating zone (57 +/- 5.8 mm Hg) than in any of the other zones of the growth plate.(7) This is due to the rich vascular supply present at the top of the zone. Considering the relatively high oxygen tension coupled with the presence of glycogen in the chondrocytes, it is apparent that aerobic metabolism with glycogen storage is occurring.
Thus the function of the proliferative zone is twofold: matrix production and cellular proliferation. The combination of these two functions equals linear or longitudinal growth. It is a paradox that while this chondrogenesis or cartilage growth is solely responsible for the increase in linear growth of the long bone, the cartilage portion of the plate itself does not increase in length. This, of course, is due to the vascular invasion that occurs from the metaphysis with the resultant removal of chondrocytes at the bottom of the hypertrophic zone, events that, in the normal growth plate, exquisitely balance the rate of cartilage production.
HYPERTROPHIC ZONE
The flattened chondrocytes in the proliferative zone become spherical and greatly enlarged in the hypertrophic zone. These changes in cell morphology are quite abrupt, and one can usually determine the end of the proliferative zone and the beginning of the hypertrophic zone within an accuracy of one to two cells. By the time the average chondrocyte reaches the bottom of the hypertrophic zone, it has enlarged some five times over what its size was in the proliferative zone.(12) The cytoplasm of the chondrocytes in the top half of the hypertrophic zone stains positively for glycogen (periodic acid-Schiff [PAS] reaction coupled with diastase digestion), but near the middle of the zone the cytoplasm abruptly loses this ability. On light microscopy, the chondrocytes in the hypertrophic zone appear vacuolated. Toward the bottom of the zone, such vacuolation becomes extensive, nuclear fragmentation occurs, and the cells appear nonviable. At the very bottom of each cell column the lacunae appear empty and are devoid of any cellular content.
On electron microscopy the chondrocytes in the top half of the hypertrophic zone appear normal and contain the full complement of cytoplasmic components. (12,21) However, in the bottom half of the zone, the cytoplasm contains holes that occupy over 58% of the total cytoplasmic column. (12) Obviously, it is holes and not vacuoles that account for the “vacuolation” seen on light microscopy. Electron microscopy also shows that glycogen is abundant in the chondrocytes in the top half of the zone, diminishes rapidly in the middle of the zone, and disappears completely from the cells in the bottom portion of the zone. The last cell at the base of each cell column is clearly nonviable and shows extensive fragmentation of the cell membrane and the nuclear envelope with loss of all cytoplasmic components except a few mitochondria and scattered remnants of endoplasmic reticulum. Clearly, the ultimate fate of the hypertrophic chondrocyte is death.
Electron micrographs reveal electron-dense granules in mitochondria of growth plate chondrocytes.(35,39) These granules are not removed by microincineration(39) (and hence, are mineral) and have been shown by direct analysis to have the characteristic radiographic spectra of calcium and phosphorus.(55) They are present in highest concentration in chondrocytes in the hypertrophic zone in the normal growth plate and are absent or greatly diminished in number in the rachitic growth plate.(49) Histochemical localization of calcium at the ultrastructural level shows the mitochondria and cell membranes of chondrocytes in the top half of the hypertrophic zone to be loaded with calcium (Fig. 2-5). (8,9) Toward the middle of the zone, mitochondria rapidly lose calcium, and at the bottom of the zone, both mitochondria and cell membranes are totally devoid of calcium. All of these studies cited above provide circumstantial evidence that mitochondrial calcium may be involved in cartilage calcification.
 |
FIG. 2-5 Electron micrographs of mitochondria from the hypertrophic zone of the growth plate stained for calcium with potassium pyroantimonate. (A) Top portion of the hypertrophic zone stained conventionally. (B) Top portion of the hypertrophic zone showing positive stain in mitochondria. (C) Middle portion of the hypertrophic zone showing beginning of depletion of calcium stain from the mitochondria. (D) Bottom of hypertrophic zone showing almost complete depletion of mitochondrial calcium. (original magnification x 82,000) |
Biochemical analyses of the hypertrophic zone indicate that this region, or at least the upper three fourths of it, is active metabolically. It contains the highest content of alkaline phosphatase, acid phosphatase, glucose-6-phosphate dehydrogenase, lactic dehydrogenase, malic dehydrogenase and phosphoglucoisomerase;(29,30) total and inorganic phosphate, calcium, and magnesium;(58) moisture and ash;(35) and lipid.(24) It contains the lowest content of hydroxyproline(24) and hexosamine(19)
Oxygen tension in the hypertrophic zone is quite low (24.3 +/- 2.4 mm Hg).(7) No doubt this low oxygen tension is due to the avascularity of the zone.
 |
FIG. 2-6 Drawing summarizing the metabolic events occurring in the various zones of the growth plate. (Brighton CT, Hunt RM: The role of mitochondria in growth plate calcification as demonstrated in a rachitic model. J Bone Joint Surg 60A:630 639, 1978) |
A summary of the metabolic events occurring in the cartilage portion of the growth plate, or, more correctly, in the proliferative and hypertrophic zones, is presented in Figure 2-6. (10) In the proliferative zone, oxygen tension is high, aerobic metabolism occurs, glycogen is stored, and mitochondria form adenosine triphosphate (ATP). Mitochondria can form ATP or store calcium, but they cannot do both at the same time.(33) Thus, ATP formation and calcium accumulation are alternative processes rather than simultaneous ones. In the proliferative zone, the energy requirement for matrix production and cellular proliferation is high, and mitochondria form ATP. In the hypertrophic zone, oxygen tension is low, anaerobic metabolism occurs, and glycogen is consumed until, near the middle of the zone, it is completely depleted. In the top half of the hypertrophic zone, mitochondria switch from forming ATP to accumulating calcium.(3) Why this switch occurs at this level in the growth plate is not entirely clear. However, both the formation of ATP and calcium accumulation are active processes requiring energy.(33) Such energy comes from the respiratory chain in the mitochondria. ATP formation requires, in addition, the presence of adenosine diphosphate (ADP), while calcium accumulation does not. It may well be that in the hypertrophic zone there simply is not enough ADP to provide for significant ATP formation. In any event, mitochondria in the top half of the hypertrophic zone accumulate calcium and do not form ATP.
In the bottom half of the hypertrophic zone, as stated above, glycogen is completely depleted. In this area of low oxygen tension, there is no other source of nutrition to serve as an energy source for the mitochondria. Since retention of calcium by mitochondria (as well as uptake of calcium) is an active process requiring energy,(34) as soon as the glycogen supply of the chondrocytes is exhausted, mitochondria release calcium. This released calcium may play a role in matrix calcification (see below).
The matrix of the hypertrophic zone, unlike the other zones, shows a positive histochemical reaction for an acid mucopolysaccharide or a disaggregated proteoglycan. Electron microscopy reveals that there is a progressive decrease in length of proteoglycan aggregates and a decrease in the number of subunits of the aggregates in the matrix as one progresses from the reserve zone through the hypertrophic zone.(15) The distance between the subunits increases at the same time. It is speculated by some that the large proteoglycan aggregates with tightly packed subunits may inhibit mineralization or the spread of mineralization, whereas smaller aggregates with widely spaced subunits at the bottom of the hypertrophic zone may be less effective in preventing mineral growth.(15) Lysozyme may be involved in the disaggregation of large proteoglycan aggregates,(28,42,51) or Iysosomal enzymes, especially neutral proteases, may degrade the proteoglycan.(49) In any event, it seems apparent that proteoglycan disaggregation or degradation must occur before there can be significant mineralization.(27,23)
The initial calcification (“seeding” or “nucleation”) that occurs in the growth plate in the bottom of the hypertrophic zone (zone of provisional calcification) does so within or upon matrix vesicles that are present in the longitudinal septa of the matrix (Fig. 2-7).(1,4,5,18)Matrix vesicles are very small structures (lOOOA-1500A in diameter) that are enclosed in a trilamellar membrane and, therefore, are produced by the chondrocyte. They occur in greatest concentration in the hypertrophic zone.(4) Matrix vesicles are rich in alkaline phosphatase,(2) and this enzyme may act as a pyrophosphatase to destroy pyrophosphate, another inhibitor of calcium phosphate precipitation.(18) Matrix vesicles begin to accumulate calcium at the same level in the middle of the hypertrophic zone at which mitochondria begin to lose calcium (Fig. 2-8).(5-9) This is circumstantial evidence indicating that mitochondrial calcium is involved in the initial calcification that occurs in the growth plate. The initial calcification in the matrix vesicles may be in the form of amorphous calcium phosphate,(43) but this rapidly gives way to hydroxyapatite crystal formation. With crystal growth and confluence, the longitudinal septa become calcified. This occurs in the bottom portion of the hypertrophic zone, a region frequently called the zone of provisional calcification.
This calcification makes the intercellular matrix relatively impermeable to metabolites. Diffusion coefficients of the various zones of the growth plate have been measured, and the hypertrophic zone has the lowest diffusion coefficient in the entire growth plate.(54) This is due primarily to the high mineral content of that zone, and suggests the following sequence of events:
1. Calcification occurs.
2. Diffusion of nutrients and oxygen to the hypertrophic chondrocyte is decreased.
3. Anaerobic glycolysis with glycogen consumption occurs until all the glycogen is depleted.
4. Mitochondria release calcium.
5. Nucleation occurs in the matrix vesicles.
6. Calcification of the matrix occurs.
 |
FIG. 2-7 Electron micrographs of matrix vesicles from the various zones of the growth plate stained for calcium with potassium pyroantimonate. (A) Proliferative zone stained conventionally. (B) Proliferative zones stained with pyroantimonate (negative stain). (C) Middle of hypertrophic zone shows clumps of calcium-antimonate complex upon or within matrix vesicles. (D) Bottom of hypertrophic zone shows crystal formation obliterating the matrix vesicle. (original magnification x 180,000). |
Thus, a cycle is established that results ultimately in the death of the hypertrophic chondrocyte (Fig. 2-9).
The functions of the hypertrophic zone seem clear: to prepare the matrix for calcification and to calcify the matrix. Although these processes are complex biophysical phenomena, it is evident from the studies cited above that we are beginning to unravel the mechanisms and factors controlling matrix calcification.
BONY COMPONENT (METAPHYSIS)
The metaphysis begins just distal to the last intact transverse septum at the base of each cell column of the cartilage portion of the growth plate (Fig. 2-10). It ends at the point at which narrowing or funnelization of the bone end ceases, that is, where the wider metaphysis meets the narrower diaphysis.(48) In the first part of the metaphysis just distal to the cartilage portion of the plate, the oxygen tension is low (19.8 + 3.2 mm Hg).(7) The low oxygen tension, as well as the rouleaux formation of the red cells frequently seen just distal to the last intact transverse septa,(6) indicates that this is a region of vascular stasis. A flocculent, electron-dense material present within the lumen of vascular sprouts invading the transverse septa may likewise indicate the presence of circulatory stasis within these vessels.(50)Also, high levels of phosphoglucoisomerase, an enzyme active in anaerobic metabolism, are found in this region and are compatible with vascular stasis(29)
In the first part of the metaphysis, the first lacuna distal to the last intact transverse septum at the base of each column of cells is, by light microscopy, either empty or contains one or more red cells. Electron microscopy shows capillary sprouts or loops lined by a layer of endothelial and perivascular cells invading the base of the cartilage portion of the plate.(50) Cytoplasmic processes from these cells push into the transverse septa and, presumably through Iysosomal enzyme activity, degrade and remove the nonmineralized transverse septa. At this same level in the metaphysis, the longitudinal septa are partially or completely calcified. Osteoblasts, which are plump, oval-shaped cells with eccentric nuclei, line up along the calcified bars. Between the osteoblasts lining the calcified bars and the capillary sprouts are seen osteoprogenitor cells, cells with little cytoplasm but with a prominent ovoid to spindle-shaped nucleus(27) This region of vascularized calcified cartilage with little or no bone formation occurring on the calcified bars is termed the primary spongiosum.(36)
 |
FIG. 2-8 Montage of electron micrographs of the hypertrophic zone shows that the calcium-antimonate staining is predominantly intracellular at the top of the zone but becomes progressively more extracellular toward the bottom of the zone. The inserts on the right are of mitochondria in chondrocytes at corresponding levels in the zone. Note the gradual loss of the calcium stain the farther down the zone the mitochondrion is located. Inserts on the left are of matrix vesicles at corresponding levels in the zone. Note the gradual accumulation of the calcium stain the farther down the zone the vesicle is located. (Brighton CT, Hunt RM: Mitochondral calcium and its role in calcification. Clin Orthop 100:406 416, 1974) |
 |
FIG. 2-9 Drawing showing events in the hypertrophic zone relating matrix calcification to decrease pO2, glycogen metabolism, and mitochondrial, calcium release (Brighton CT, Hunt RM: The role of mitochondria in growth plate calcification as demonstrated in a rachitic model. J Bone Joint Surg 60A:630 638, 1978) |
 |
FIG. 2-10 Drawing of the metaphysis showing the interlocking of the primary and secondary spongiosa. (Brighton CT: Structure and function of the growth plate. Clin Orthop 136:23-32, 1978) |
A short distance (within a cell or two) further down the calcified longitudinal septa, the osteoblasts begin laying down bone (termed endochondral ossification, i.e., bone formation within or upon cartilage). The further down or into the metaphysis one progresses, the more bone is formed on the calcified cartilage bars. At the same time, the bars gradually diminish in thickness until they disappear altogether. This region, where bone is laid down on calcified cartilage bars, is termed the secondary spongiosum.(36)
Still further down in the metaphysis, the fiber bone that was formed originally is replaced with lamellar bone. This gradual replacement of the calcified longitudinal septa with newly formed fiber bone, as well as the gradual replacement of fiber bone with lamellar bone, is termed internal or histologic remodeling. (32)
Large, irregularly shaped cells with foamy, eosinophilic cytoplasm and one or more nuclei each containing several nucleoli are evenly distributed throughout the entire metaphysis except in the primary spongiosum. These osteoblasts are also seen subperiosteally around the outside of the metaphysis where it diminishes in diameter to meet the diaphysis. This narrowing or funnelization of the metaphysis is termed external or anatomic remodeling.(32)
The functions of the metaphysis therefore, are vascular invasion of the transverse septa at the bottom of the cartilaginous portion of the growth plate, bone formation, and remodeling, both internal and histologic (removal of calcified cartilage bars and replacement of fiber bone with lamellar bone) and external or anatomic (funnelization of the metaphysis).
FIBROUS AND FIBROCARTILAGINOUS COMPONENTS
Encircling the typical long-bone growth plate at its periphery are a wedge-shaped groove of cells, termed the ossification groove, and a ring or band of fibrous tissue and bone, termed the perichondrial ring(Fig. 2-11). Ranvier,(46) the first to describe these structures, concentrated his study on the cells in the groove, which is now named after him. LaCroix(31) studied the perichondrial ring in detail, and this structure is frequently named after him. Although it is true that the ossification groove and the perichondrial ring are simply different parts of the same structure, they do have different functions, and for that reason alone it is advantageous to consider them as separate and distinct entities. These structures will be described first as they are found in the typical long-bone growth plate (distal femur) and then as they exist in a somewhat different form in the femoral capital growth plate.
 |
FIG. 2-11 Photomicrograph of the periphery of the distal femoral growth plate of a 14-day-old rat shows the ossification groove of Ranvier (A) and the perichondrial ring of LaCroix (B). (H&E x loo) (Brighton CT: Clinical problems in epiphyseal plate growth and development, pp 107-113. AAOS Instructional Course Lecture, vol XXIII, p 107. St Louis, CV Mosby, 1974) |
The ossification groove contains round to oval cells that, on light microscopy, seem to flow from the groove into the cartilage at the level of the beginning of the reserve zone. For that reason, and since these cells avidly incorporate tritiated thymidine, it appears that the function of the groove of Ranvier is to contribute chondrocytes to the growth plate for the growth in diameter, or latitudinal growth, of the plate.(52) In a recent, definitive study using electron microscopy and autoradiography, three groups of cells were identified in the ossification groove: a group of densely packed cells that seemed to be progenitor cells for osteoblasts that form the bony band in the perichondrial ring; a group of undifferentiated cells and fibroblasts that contribute to appositional chondrogenesis and, hence, growth in width of the growth plate; and fibroblasts amid sheets of collagen that cover the groove and firmly anchor it to the perichondrium of the hyaline cartilage above the growth plate.(57)
 |
FIG. 2-12 Photomicrograph of the periphery of the proximal femoral growth plate of a 14-day-old rat shows the fibrocartilaginous structure that replaces the groove of Ranvier and perichondrial ring in other growth plates. (H&E x 100) |
The perichondrial ring is a dense fibrous band that encircles the growth plate at the bone-cartilage junction and in which collagen fibers run vertically, obliquely, and circumferentially.(45) It is continuous at one end with the group of fibroblasts and collagen fibers in the ossification groove and at the other end with the periosteum and subperiosteal bone of the metaphysis. In rodents, rabbits, and dogs, the innermost layer of the perichondrial ring consists of bone that may or may not be attached to the subperiosteal bone of the metaphysis. This cylindrical sheath of bone may not be present in all species at all ages in all growth plates. For instance, it is not present in the proximal femur in the human at any age. ” Whether or not bone is present in the perichondrial ring, there is no doubt that the ring provides mechanical support for the otherwise weak bone-cartilage junction of the growth plate (17,47,52)
Hence the function of the ossification groove is to provide chondrocytes for the growth in width of the growth plate, and the function of the perichondrial ring is to act as a limiting membrane that provides mechanical support to the growth plate.
In the femoral capital growth plate, the functions of the ossification groove and the perichondrial ring are the same as in any typical long-bone growth plate, but the structure of these peripheral tissues is quite different. Instead of a rather distinct ossification groove and perichondrial ring, these two structures are replaced by one structure that consists of fibrocartilage in the area that is occupied by the groove of Ranvier and the perichondrial ring in other growth plates (Fig. 2-12). This structure apparently has the same functions as the groove of Ranvier and the perichondrial ring, that is, to provide for latitudinal growth of the growth plate (top portion of the fibrocartilaginous structure) and to provide mechanical support to the growth plate (remainder of the fibrocartilaginous structure).(17)
SECTION TWO
DIAPHYSEAL BONE FORMATION
ARTHUR W. FETTER
One of the earliest indications that the cartilage model of a long tubular bone is about to be replaced is the appearance of a thin collar (ring or sleeve) of osseous tissue around the middle. The formation of the osseous collar is induced when the cartilage cells in the area mature and hypertrophy, and the matrix they have produced becomes mineralizable. The collar of bone, which represents the first stage in the development of the cortex of the evolving bone, is formed through intramembranous ossification from osteoblasts in the inner or osteogenic layer of the perichondrium. This fibrous tissue layer, because of its location, should be called periosteum. The cortical shell consists of a loosely woven matrix with more cells per unit area than that which occurs in mature bone.
The formation of the periosteal osseous collar is rapidly followed by the extension of vascular buds from the periosteum through the cortical shell into the cartilaginous area. This process is induced by the degeneration and death of cartilage cells. These primitive vessels enter the degenerating cartilage, bringing with them mononuclear cells and mesenchymal elements, which give rise to the chondroclasts, osteoclasts, and osteoblasts. These cells are essential in the process of enchondral ossification and the formation of the hematopoietic marrow of the evolving bone.
As the diaphysis elongates, the cortical shell of bone continues to develop adjacent to the growth plate and remains at, or slightly beyond, the level of the zone of hypertrophied cartilage cells, providing structural support for the cartilaginous epiphysis. This extension of the cortical shell forms a three-dimensional cup and is called Ranvier’s ossification groove (encoche deRanvier). In order to maintain the funnel shape of the bone as it grows in length, remodeling of the metaphysis begins almost as soon as any bone is formed.
During the rapid advance of enchondral ossification toward the epiphyseal ends of the elongating young bone, growth is also occurring subperiosteally in the diaphysis. The periosteum becomes quite thick, and spicules of new bone are deposited more or less perpendicularly between the cambium layer of the periosteum and the original cortical shell. The matrix of the rapidly deposited bone is loosely woven, resembling burlap, and contains many cells per unit area of bone. As cortical growth in the area of the diaphysis slows, osteoblasts line up on the surface of the bone spicules and slowly deposit lamellar bone in the form of an “inlay” into the spaces between the trabeculae. This filling between the trabeculae results in the formation of a solid cortex. At this stage, the cortex consists of a mixture of woven fiber bone with its haphazard fibrillar arrangement and numerous osteocytes, and the lamellar bone with a parallel arrangement of collagen fibers and fewer osteocytes. The inlay bone has an osteonal appearance, but true osteons are formed as refill after osteoclasts have cut a hole in cortical bone. Therefore, the inlay bone does not qualify as true osteonal bone.
SECTION THREE
CORTICAL REMODELING
ARTHUR W. FETTER
Once a cortical surface is formed, layer after layer of bone is deposited on the surface in the form of coarse lamellar bone. Since this bone is not initially deposited along lines of stress, but rather in response to vascular patterns and growth patterns, remodeling must occur. This remodeling is accomplished by osteoclasts, the number and activity of which are influenced by circulatory, metabolic, and mechanical factors.(59) The initial event in remodeling is the removal by osteoclasts of matrix that was previously deposited by osteoblasts. This occurs through the action of a “cutting cone” of osteoclasts, which progresses more or less longitudinally along the developing shaft of the bone. The cutting cone advances along the course of the vessel, producing a resorption cavity (Fig. 2-13, A). Following along behind the cutting cone, osteoblasts become aligned on the walls of the resorption cavity and secrete a layer of mucopolysaccharides on the surface of the cavity, which is referred to as a cement or reversal line. Successive generations of osteoblasts then produce layers of bone that fill in the resorption cavity in centripetal fashion, leaving a small central canal that contains vessels and nerves. This process results in the production of an osteon or haversian system, which consists of the central canals with their blood vessels, canaliculi, and the concentric lamellae of bone (Fig. 2-13, B). The canaliculi contain osteocytic processes during life and radiate from the central canal, thereby interconnecting the osteocytic lacunae. Thus, each haversian system or osteon is a single metabolic unit nourished by the vessel in the central canal, with nourishment proceeding outward through the canaliculi (Fig. 2-14).
 |
FIG. 2-13 (A) Numerous resorption cavities in various stages of refill in cortical bone. Note recently formed resorption cavities (short arrows) and others that are partially filled by osteonal bone formation (long arrows) The dark circumferential bands within the resorption cavities are osteoid seams of the developing osteon. The mineralized section of bone is stained with Goldner’s modified trichrome stain. (B) Mature cortical bone characterized by fully developed osteons with minimal resorptive activity. The mineralized section of bone is stained with Goldner’s modified trichrome stain. |
 |
FIG. 2-14 A single osteon characterized by a central canal (C) osteocytic lacunae (O), and osteocytic processes within canaliculi (arrows). The mineralized bone section is stained with basic fuchsin. |
 |
FIG. 2-15 Cortical bone consisting of numerous osteons (O) and interstitial fragments (F). Unstained section of mineralized bone. |
As cutting cones remodel bone, they do so with a “skew” determined by mechanical stresses. Therefore, the cutting cone may cross osteonal lines, removing portions of several osteons. When these resorption cavities are refilled, portions of the original osteons are left behind. After several waves of such activity, numerous interstitial fragments remain. Since a cement or reversal line is deposited following the formation of the cavity, the interstitial fragments are not directly connected to any haversian blood supply (Fig. 2-15). With the passage of years and many waves of remodeling activity, the number of interstitial fragments becomes greater and greater. Volkmann’s canals course transversely through the cortex, connecting adjacent haversian systems and providing intercommunication between the medullary and the periosteal blood supply. These canals are not surrounded by concentric layers of bone, as are the osteons.