Me: I wanted to make this post be about using surgery to correct for spinal deformities. In effect, the rod implanted into the vertebrate to stop the curvature of the spine and relieve much pain will also increase height.
I found this article HEY Clinic For Spine & Surgery at Raleigh, NC where a spine surgeon talks about using a new 4-rod implant to make a patient who already had implants in her back stronger and more durable since her current rods have broken apart..
The Hey Clinic for Scoliosis and Spine Surgery
This is where Dr. Hey shares his thoughts regarding recent patients he has cared for, and shares photos and case summaries to benefit patients, their families and friends, other physicians, medical students, residents, and fellows. Dr. Hey works at the Hey Clinic for Scoliosis and Spine Surgery, Raleigh, NC USA http://www.heyclinic.com.
FRIDAY, SEPTEMBER 14, 2007
 Hey Clinic Sep 13 2007 AM Surgery: New “QUAD ROD” technique for stabilizing thoracic kyphotic fracture with history of rod breakage.
Hey Clinic Sep 13 2007 AM Surgery: New “QUAD ROD” technique for stabilizing thoracic kyphotic fracture with history of rod breakage.
Yesterday morning, September 13th 2007, we helped a Nancy, a 75 yo woman who had a T12 severe wedge fracture above a previous fusion which caused myelopathy and severe pain. This was fixed using a laminectomy, and extension instrumentation and fusion. Postoperatively, she had trouble with rod breakages at that high load area around T12, with 2 rod construct, and then 3 rod construct. She how presented with recurrent rod breakage at that same T12 area, breaking both rods, and breaking conectors for the triple rod, resulting in recurrent kyphosis and pain. Given the amount of wedging at T12, we had discussed possibility of fixing this problem with an anterior/posterior procedure, removing body of T12 and replacing the vertebra with a strut expandable cage with graft, then instrumenting posteriorly. However, that is a very big operation, which involves having to take down diaphragm, etc., and Nancy was not interested in that at all. So, for the past couple of months, I have been working on several different engineering designs to make a stronger construct across this junction, “playing” with my set of Synthes “erector set” tools, and trying to come up with a new design which would be at least ten times stronger than the last one, but also be low profile enough that it would not cause problems with soft tissue prominence.
What seemed to be the best solution is a new surgical technique that I call the “Quad Rod”. Instead of just having 2 rods going across the area of the fracture, there are actually four rods, all closely coupled to each other with very strong rod to rod connecters. The combination of this second rod on each side closely coupled to the main rod means that there is major improvement in bending and twisting strength and rigidity, while still keeping a low profile instrumentation, while leaving the lateral “gutter” over the transverse processes wide open for BMP and bone graft.
Over the past couple months, I have done a bunch of different permutations of the “Quad Rod” on the spine model, and also experimented with other combinations including a 6 rod construct, which proved to be very strong, but very bulky. I also got a chance to try a small version of the Quad Rod unilaterally on a surgery a couple weeks ago which went well, and helped me think through some of the complexities of the rod insertion.
For my resident and fellow and younger spine surgeon readers, let me go over a few basic points.
1. Rods and/or screws are not meant to be able to withstand a lifetime of loading for most normal-sized people: they are meant to hold things in position hopefully long enough for the bone to heal, forming a fusion along the spine. This fusion can be thought of as “cement” that very slowly “hardens” around the metal superstructure, forming a very solid construct. However, the bone can take up to a year or even more to completely heal, especially in older patients who have weaker bone that does not make bone as quickly. If the bone does not heal, it is possible that the rods could break, or that the screws could loosen in the bone, and start to “toggle”. This could cause pain and deformity.
2. Whenever you face a revision instrumentation case, you always want to be thinking about making your new construct much stronger than the old one, while trying to get the bone to heal quicker using biological enhancers like bone morphogenic protein (BMP) and local or autologous bone graft. My military analogy here is this: If you get beaten in battle with 20 guys, don’t go back the next time with 20 or 21 guys —-> bring 100+ guys the next time, maybe with fire power from aircraft and a tank or two!
In this particular case, my first revision instrumentation used a triple rod technique with BMP, which had been my rock-solid revision instrumentation technique for broken rods, which had worked without fail for past 3 years or so without fail… Until Nancy broke the Triple Rod a couple months ago! So this time I am calling out the Marines, Air Force, Army, Navy and the Six Million Dollar Man! Here are the things I planned to do, and did differently with this revision:
1. Replace the screws above and below the unstable fracture with new screws, at least 1mm in diameter larger than the last ones. Putting in new screws here helps since the old ones had a lot of “cycles of load” on them and could break. 1mm larger diameter for each of these screws also makes the screw much stronger — the strength of the screw goes up as the 4th power of the diameter! (That’s like way bigger than double, or square or triple). So, for example, if you were to double the diameter of the screw, the strength would go up 16 time!
2. Put pedicle screws into the body of T12, where the fracture occurred. While I could not do this originally when the fracture occurred, since the body was “smashed”, now that it has been a year or more since her original fracture, I had hoped that the bone would have healed. Much to my delight today, I found that the bone had healed. It was still very tricky to get the screws placed, given previous laminectomy and scar, etc, but thankfully I got in 2 very solid screws at T12. This extra vertebral body support directly adjacent to where the fracture was unstable helped tremendously to improve the strength of the overall construct.
3. Stronger Rods. Thankfully, Synthes just recently released a new Titanium Alloy rod which is much stronger than the old rod, but is the same 7mm diameter. One of the fun things that occurred in this particular case was my interactions not only with Nancy, but with Nancy’s husband, Bob, who has a phenomenal background in metallurgy and engineering. One of Bob’s initial suggestions for this last revision was to use larger diameter rods, which from an engineering standpoint makes a lot of sense, but from a biologic standpoint doesn’t work as well, since the rods would become prominent. It would also require all of the screws and other connectors to be re-machined, and then retested. The best we could do was to get a stronger rod, but in the same diameter by changing the titanium alloy.
4. “HEY QUAD ROD”. This is one strong construct. The close coupling of 2 rods almost right next to each other with three encasing titanium block sleeves, which are then locked to each other with set screws makes for an incredible “I-Beam” that resists bending and twisting greatly. We recently received a grant, and are working with Professor Mazzolini and others at NC State Department of Mechanical Engineering to study the strength of some of these new constructs using computer models and lab testing. This “Quad Rod” is tough to put together, but once together is very low profile, and very strong. I have a bunch of tips that make it work very well. I used the new Quad Rod with the Synthes USS Titanium system, which has a special cap and nut locking system that locks the rod to the screw. One of the troubles you may have trying to do the Quad Rod with another system is that the screw diameter may be too large to allow the second joining rod to fit with the rod to rod connector. The rod to rod connector is something that other systems may have, which is used usually for doing extension instrumentations, where one rod is added onto another rod. In this case, I actually used a total of 5 rod to rod connectors on each side, and 10 altogether: three are used around the apex of the fracture, with the middle one right over the T12-L1 toggle point, and then one above at T11-T12 interspace, and L1-L2 interspace just below the apex of the “toggle”. The other 2 rod to rod connectors are placed at the top and bottom of the whole section of rod I replaced, which were down at L2 and up at T6 on each side. It turns out that the rod to rod connectors are almost the perfect length to “fill” the interspace between each of the pedicle screws, creating an additional thick “sheath” around the rod for extra bending resistance. The closely coupled rod next to the main rod provides additional bending and twisting support as a very tightly joined and/or cross-linked rod.
5. Additional cross-link between L and R rods just above the Quad Rod. There was too much fusion mass below the Quad Rod to put another cross-link, plus the large fusion mass below worked like a “cross link”.
6. Very aggressive cleanout of the pseudarthrosis at T12-L1, and the lateral “gutter” on either side, out over some of medial rib on both sides. This decoricated old fusion mass made a great new organic “bed” for two long strips of Medtronic Bone Morphogenic Protein (BMP) soaked sponges, followed by a layer of local bone graft, followed by a thick layer of allograft finely morselized chips.
Overall, the surgery went very well, taking right around 4 hours total.
I was able to accomplish all six of the steps above, although there were some real “fiddle factors” that needed to be dealt with. Here are a few pearls:
- Your replacement long rod needs to be just the right length to connect between the very top and bottom connectors, but not significantly longer. When you go to insert the final construct, you need to slide it in one end, and then reduce it into the screw channels above, and then slide it up and into the rod to rod connectors at the very top.
- Keeping those top and bottom connectors a little bit loose so they can rotate helps to get the new rod into the hole, and then rotated down into position and into the screw slots.
- Measure your “partner rod”, the second rod on each side to bridge across 3 interspaces around the max stress point, with middle rod to rod connector over where the rods broke the last time.
- Bend the rod in that area for both rods as little as possible, to avoid weakening the rod, and also to allow the rod to rod connectors to slide easily.
- Attach the “partner rod” before inserting the overall construct, and put it medial to the main rod, with pedicle screw openings also facing medial. You will not be able to slide in partner rod when the first rod is in place. Placing it medial leaves the lateral gutter totally free for BMP and bone graft.
- Mark the main rod with a pen where the 3 rod to rod connectors need to go to fall between the pedicle screws.
- Put the middle of the 3 connectors on the partner and main replacement rod first, then slide the other two connectors over either end. Much easier than trying to guide the smaller partner rod through 3 connectors.
- Insert the longer replacement rod at one end of the distal connectors first, as mentioned above, and then slide it into the upper connector, taking advantage of the rod to rod connector’s ability to rotate 90 degrees, and then down into position next to the screws.
- Use the “Pursuader” to push the rod into the pedicle screws — it even works across the two rod construct! Tighten your set screws a little bit before you “pursuade” the double-rod construct into the screw slot.
- As you are tapping the cap down over the main rod, there is very little space between the 2 rods — back off the compressor on the Pursuader a little bit, and the narrow “skirt” of the cap will go right between the 2 rods, and lock into position. Yahoo!
- Torque down your set screws before tightening your nuts on top of the caps, for maximum strength.
- Do thorough cleanout of lateral gutter and takedown of pseudarthrosis.
- Strongly consider prior to placing rods putting additional screw points of fixation around the area of the “toggle” as I did, by putting T12 screws into old fractured vertebra. The more points of fixation you have, the better the load is shared to the spine, with less bending moment between screws.
- Cut the BMP sponges into 2 longitudinal strips, and lay them down as a floor to the “gulley” over the transverse processes, ribs, and old fusion mass.
- Undercut the paraspinal muscle flaps to allow for tension-free fascial closure at the end of surgery.
We will be studying this and other constructs in the future.
I encourage you to spend a lot of time “playing” with this and other constructs, using the plastic spine models with points of fixation, but also experimenting with other potential constructs as a pure erector set, to understand the possibilities. I see some possible very interesting constructs by joining 2 rod to rod connectors serially together, forming a double hinge. This allows you to have a “Quad Rod” where the rods are further apart, thereby potentially creating a better “I Beam” , by increasing the distance between the 2 beams. However, there are prominence problems, and the need for 2 connectors connected by a short intermediate rod I think is not half as strong as having 2 rods locked side by side. Perhaps a wider rod to rod connector would be a possibility, to allow the second rod to have more flexibility as to where it lies, and to potentially increasing the distance between the rods to increase strength.
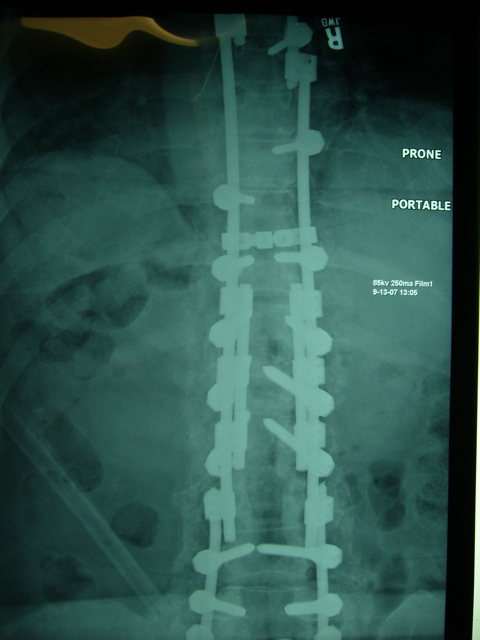
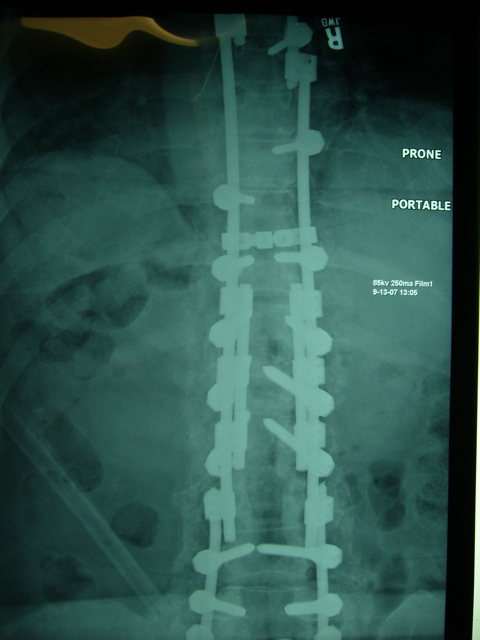
Below are some pictures of our performance of our first real “Hey Quad Rod”.
I am happy to say that we got an excellent correction of her deformity, and we still have load sharing on the middle column anteriorly. However there is a big “divit” in the anterior portion of T12, which would have been nice to “fill in” with an anterior strut, but too invasive for Nancy. Our posterior Quad Rod tension band, combined with our “quick dry” BMP/bone graft combination, combined with even stricter postoperative patient restrictions for bending and lifting should hopefully lead to a long-term fix for Nancy.
This evening she was looking great in ICU, ready to get up and be probably 3-4 inches taller.
I hope these notes and pictures are helpful to my fellow surgeons out there. Please do not hesitate to call or email me if you have further questions or thoughts.
My email is “hey” at heyclinic.com, and my phone is available through website http://www.heyclinic.com.
Lloyd A. Hey, MD MS
Hey Clinic for Scoliosis and Spine Surgery
Raleigh, NC USA
http://www.HeyClinic.com