A sesamoid is a bone formed within a tendon or muscle while we’re looking for is more interosseous chondroification(the formation of new cartilage tissue within the bone) or probably maybe even first interosseous epithelialification as you might need to transition mesenchymal to epithelial tissues first.
Coincident development of sesamoid bones and clues to their evolution.
“Sesamoid bones form within tendons in regions that wrap around bony prominences. They are common in humans but variable in number. Sesamoid development is mediated epigenetically by local mechanical forces associated with skeletal geometry, posture, and muscular activity. In this article we review the literature on sesamoids and explore the question of genetic control of sesamoid development. Examination of radiographs of 112 people demonstrated that the relatively infrequent appearances of the fabella (in the lateral gastrocnemius tendon of the knee) and os peroneum (in the peroneus longus tendon of the foot) are related within individual. This finding suggests that the tendency to form sesamoids may be linked to intrinsic genetic factors. Evolutionary character analyses suggest that the formation of these sesamoids in humans may be a consequence of phylogeny. These observations indicate that variations of intrinsic factors may interact with extrinsic mechanobiological factors to influence sesamoid development and evolution.”
“As many as 42 sesamoid bones can be found in some individuals. Mechanically, sesamoid bones serve to protect the tendon from damage and, in some cases, increase the efficiency or mechanical advantage of their associated muscle.”
“Most sesamoid bones in humans are 5 to 10 mm in diameter or smaller and are present in 1 to 100% of individuals.”
“Tendon chondrometaplasia[tendon turns into cartilage] and sesamoid bones tend to develop within tendons in areas that experience both tensile strain and hydrostatic compressive mechanical stresses.”<-So tendonous tissue may help form neo growth plates. Tendon enthesis attach into the bone. Tendon is capable of undergoing chondrometaplasia. So potentially you could form neo growth plates at these tendon entheses. Originally I thought that ligament enthesis had more potential for neo-growth plate formation but tendon enthesis may have potential too.
” fibrous tendon tissue can form regions of fibrocartilage in areas that wrap around bony prominences (fibrocartilage is a tissue whose phenotype is intermediate between fibrous and cartilaginous tissue, consisting of chondrocytes embedded in aligned bundles of type I collagen)”
“compression loading and treatment with transforming growth factor beta (TGF-β) each resulted in upregulation of aggrecan and biglycan synthesis in fetal bovine tendon, suggesting that one aspect of the response of cells to compressive load is increased TGF-β synthesis which, in turn, stimulates synthesis of extracellular matrix proteoglycans and leads toward fibrocartilage formation. The process of fibrocartilaginous metaplasia in tendons, which is a direct response to an altered mechanical loading environment, appears to represent an intermediate step in the formation of a sesamoid cartilage.”
Sesamoid bones:
Their position won’t help you grow taller but they could if they were in the articular cartilage. Maybe if tendonous tissue was inserted in the articular cartilage.
“Hox A11, had profound effects on the developing mouse skeleton, including abnormal sesamoid bone development in both the forelimbs and hindlimbs.”
How might we turn tendons(and especially tendenous enthesis) into cartilage tissues. What if we form a sesamoid bone within the enthesis?
“Ectopic chondrogenesis and ossification were observed in a degenerative collagenase-induced calcific tendinopathy model and to a lesser extent, in a patellar tendon traumatic injury model. We hypothesized that expression of bone morphogenetic protein-2 (BMP-2) contributed to ectopic chondrogenesis and ossification. This study aimed to study the spatial and temporal expression of BMP-2 in our animal models.
Seventy-two rats were used, with 36 rats each subjected to central one-third patellar tendon window injury (C1/3 group) and collagenase-induced tendon injury (CI group), respectively. The contralateral limb served as controls. At week 2, 4 and 12, 12 rats in each group were sacrificed for immunohistochemistry and RT-PCR of BMP-2.
For CI group, weak signal was observed at the tendon matrix at week 2. At week 4, matrix around chondrocyte-like cells was also stained in some samples. In one sample, calcification was observed and the BMP-2 signal was observed both in the calcific matrix and the embedded chondrocyte-like cells. At week 12, the staining was observed mainly in the calcific matrix. Similar result was observed in C1/3 group though the immunopositive staining of BMP-2 was generally weaker. There was significant increase in BMP-2 mRNA compared to that in the contralateral side at week 2 and the level became insignificantly different at week 12 in CI group. No significant increase in BMP-2 mRNA was observed in C1/3 group at all time points.
Ectopic expression of BMP-2 might induce tissue transformation into ectopic bone/cartilage and promoted structural degeneration in calcific tendinopathy.”
“the presence of chondrocyte phenotype and ectopic ossification in a collagenase-induced patellar tendon injury model”
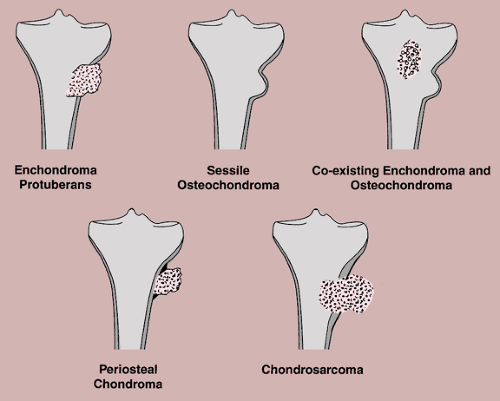
Here’s potential chondrogenic lesions: