Biochemical and physical signal gradients in hydrogels to control stem cell behavior.
“Cells continuously receive biochemical and biophysical stimuli from their microenvironment. These environmental stimuli drive cellular behavior and function during development and tissue regeneration.”<-We can alter the microenvironment via mechanical means to alter cellular behavior and ideally create neo-growth plates.
“Cell interactions with the extracellular matrix (ECM) and physical signals such as matrix rigidity and mechanical stimuli can also have strong effects on cellular phenotype and tissue formation.”<-The bone ECM likely has a strong negative regulatory effect on neo-growth plate formation. But we can alter the bone ECM via mechanical means as well.
“[we prepared] HP-ALG hydrogels with incorporated gradients of heparin binding growth factors BMP-2, a potent osteogenic growth factor, and TGF-β1, a chondrogenic growth factor, in opposite directions. When the concentration of growth factors in segments of gradient HP-ALG hydrogels was quantified, linear gradient distributions of BMP-2 and TGF-β1 in opposite directions were observed”
“As the BMP-2 concentration increased, ALP expression significantly increased along the BMP-2 gradient. In contrast, GAG production of encapsulated hMSCs significantly increased as the TGF-β1 concentration increased”
Regulation of Stem Cell Fate in a Three-Dimensional Micropatterned Dual-Crosslinked Hydrogel System.
“By manipulating micropattern size while keeping the overall ratio of single- to dual-crosslinked hydrogel volume constant, the physical properties of the micropatterned alginate hydrogels are spatially tunable. When human adipose-derived stem cells (hASCs) are photoencapsulated within micropatterned hydrogels, their proliferation rate is a function of micropattern size. Additionally, micropattern size dictates the extent of osteogenic and chondrogenic differentiation of photoencapsulated hASC. The size of 3D micropatterned physical properties in this new hydrogel system introduces a new design parameter for regulating various cellular behaviors, and this dual-crosslinked hydrogel system provides a new platform for studying proliferation and differentiation of stem cells in a spatially controlled manner for tissue engineering and regenerative medicine applications.”
“cell behaviors such as differentiation and proliferation are known to be affected by cell cluster size”
” micropattern size dictated the extent of osteogenic and chondrogenic differentiation of photoencapsulated hASC.”
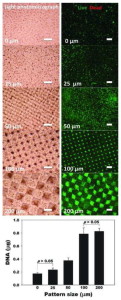
“the aggrecan expression of hASCs gradually increased as the micropattern size increased”<-But some markers increased at 200 micrometers so the optimal micropattern size should be around 100-200 micrometers.
HEre’s a visualization of micropatterns:
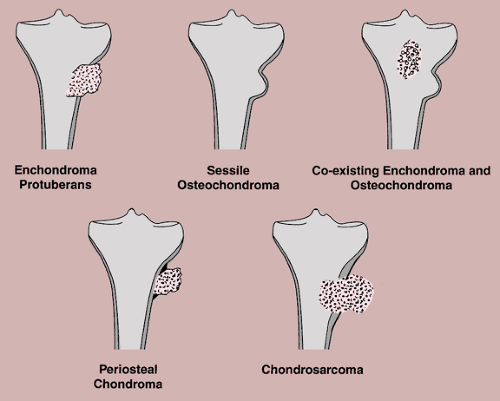
“The reconstruction of musculoskeletal defects is a constant challenge for orthopaedic surgeons. Musculoskeletal injuries such as fractures, chondral lesions, infections and tumor debulking can often lead to large tissue voids requiring reconstruction with tissue grafts. Autografts are currently the gold standard in orthopaedic tissue reconstruction; however, there is a limit to the amount of tissue that can be harvested before compromising the donor site. Tissue engineering strategies using allogeneic or xenogeneic decellularized bone, cartilage, skeletal muscle, tendon and ligament have emerged as promising potential alternative treatment. The extracellular matrix provides a natural scaffold for cell attachment, proliferation and differentiation. Decellularization of in vitro cell-derived matrices can also enable the generation of autologous constructs from tissue specific cells or progenitor cells. Although decellularized bone tissue is widely used clinically in orthopaedic applications, the exciting potential of decellularized cartilage, skeletal muscle, tendon and ligament cell-derived matrices has only recently begun to be explored for ultimate translation to the orthopaedic clinic.“
“ECM is a product of cells that functions to maintain tissue and organ structure, organization and function. It is a complex network of proteins and polysaccharides forming an intricate meshwork within tissue that interacts with the resident cells to regulate cell behavior, such as migration, proliferation and differentiation. The ECM exists in a state of dynamic equilibrium with its resident cells and is constantly being built, reshaped and degraded in response to changing environmental conditions and to cellular, tissue and organ demands”<-So we should try to alter the bone ECM to be more favorable to cartilaginous tissues.
“Fracture healing requires an intricate and well-organized series of cellular and molecular events. It involves interactions between cortical bone, the periosteum, undifferentiated fascial tissue surrounding the fracture and the bone marrow. Fracture healing is divided into three stages: inflammation, repair and remodeling. After an injury, there is initial bleeding from the damaged bone ends and surrounding tissue resulting in the formation of a hematoma, which provides a source of hematopoietic cells capable of secreting growth factors. The invasion of inflammatory cells, fibroblasts, mesenchymal cells, and osteoprogenitor cells at the fracture site forms granulation tissue around the fracture ends{To induce neo-growth plates we have to allow this invasion}. Fractures that are anatomically aligned with absolute stability, such as those surgically repaired with compression plates, undergo primary bone healing or Haversian remodeling, in which there is direct osteonal healing within the cortex by intramembranous ossification”
” in closed reduced fractures, secondary bone healing occurs with the formation of a bridging soft callus consisting of cartilage tissue connecting the fracture ends. Over time, bone formation occurs under the periosteum and calcification of cartilage results in the formation of hard callus or woven bone by endochondral ossification”
“injuries that penetrate the subchondral bone often result in the formation of fibrocartilage which is biomechanically insufficient compared to hyaline cartilage, resulting in further damage over time”
“the peak force transmitted through the Achilles tendon while running is 9 kN, which is about 12.5 times the body weight”