Update: I’m still working on a new non-LSJL method.
I don’t believe that chocolate can make you wildly taller but it tastes good. I also think the optimal diet for longitudinal bone growth varies on developmental stage.
Chocolate and Chocolate Constituents Influence Bone Health and Osteoporosis Risk
“Bone loss resulting in increased risk of osteoporosis is a major health issue worldwide. Chocolate is a rich source of antioxidant/anti-inflammatory flavonoids as well as dietary minerals with the potential to benefit bone health. However, other chocolate constituents such as cocoa butter, sugar and methylxanthines may be detrimental to bone. Human studies investigating the role of chocolate consumption on serum bone markers and bone mineral density (BMD) have been inconsistent. A contributing factor is likely the different composition and thereby, nutrient and bioactive content amongst chocolate types. White, followed by milk chocolate, are high in sugar and low in flavonoids and most minerals. Dark chocolate (45-85% cocoa solids) is high in flavonoids, most minerals, and low in sugar with ≥70% cocoa solids resulting in higher fat and methylxanthine content. The aim of this review was to examine the relationship between consuming chocolate, its flavonoid content, and other chocolate constituents on bone health and osteoporosis risk. Studies showed postmenopausal women had no bone effects at moderate chocolate intakes; whereas, adolescents consuming chocolate had greater longitudinal bone growth{whether this fact can be used for any purpose though….}. Based on flavonoid and mineral content, unsweetened cocoa powder appeared to be the best option followed by dark chocolate with higher cocoa content in terms of supporting and preserving bone health. Determining dietary recommendations for chocolate consumption regarding bone health is important due to the growing popularity of chocolate, particularly dark chocolate, and an expected increase in consumption due to suggestions of health benefits against various degenerative diseases.”
“Diets that promote bone health have mainly focused on increasing Ca and
vitamin D consumption, but there is growing interest in phytochemicals[chemicals produced by plants]”
“Dietary polyphenols consist of a large group of plant-derived secondary metabolites
divided into four different classes, one of which is the flavonoids (diphenylpropanes C6-C3-C6).
Flavonoids contain several classes of bioactive compounds. There is evidence
that intake of specific flavonoids may promote bone health including: soybean isoflavones (e.g. genistein{genistein may increase HSP90 levels and HSP90 definitely affects the growth plate but in some instances it stimulated growth and some incidences suppressed it} and daidzein), flavonols (e.g. aglycone quercetin{quercetin definitely impacts factors involved in longitudinal bone growth but the evidence is not that strong}) found in plums, and flavonones (e.g. hesperidin) found in citrus pulp and juice. Another food source noted for its flavonoid content is chocolate. Cocoa, a major constituent in chocolate, has the highest flavanol content of all foods on a per-weight basis and contributes to greater total dietary intake of flavonoids than tea, fruits, and vegetables ”
“Both animal models and human clinical trials have reported an inverse association
between reactive oxygen species (ROS) and bone health. ROS can affect bone cells in
various ways including stimulation of osteoblast apoptosis and senescence and by upregulation of receptor activator of nuclear factor kappa-B ligand (RANKL) to activate osteoclast differentiation and bone resorption”<-I think though there is a role for ROS. It’s just too many is a bad thing. And bone can be inhibitory towards longitudinal bone growth but it’s degradation of bone(bone turnover) not degradation of bone building cells that would be beneficial.
“catechins preserved bone-forming osteoblasts by exerting anti-inflammatory actions”
” In a randomized, double-blinded placebo-controlled study, pre-pubertal (n=149, age 6.6-9.4 years) girls consumed two Ca-supplemented food products daily to achieve a Ca dose of 850 mg/d. Results showed consuming Ca-supplemented chocolate bars, cakes or cocoa beverages for 48 weeks significantly increased height and bone mass acquisition in the radius and femur”
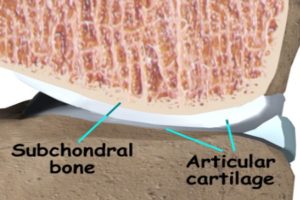
“Feeding murine dams chow diet supplemented with 400 mg unsweetened chocolate during pregnancy and lactation resulted in progeny with significantly shortened forefeet and hindlimbs. Vascular endothelial growth factor (VEGF), which plays a role in ontogenesis and longitudinal bone growth related to angiogenesis in the epiphyseal growth plate, was significantly reduced in the femora of immature (age 4-weeks old) mice pups exposed perinatally to chocolate. A follow-up study investigating the relationship of the chocolate constituent, catechins on angiogenesis and bone mineralization in the progeny of murine dams fed chocolate showed a negative correlation between embryo tissue epigallocatechin concentration and mean number of newly-formed blood vessels. Crystallinity of compact bone of diaphyses was 17% greater and femoral epiphyseal cancellous bone was 30% greater in pups age 4-weeks old exposed perinatally to chocolate compared to pups from control dams. The authors suggested anti-angiogenic activity of chocolate catechins disturbed the processes of bone elongation and mineralization “<-so chocolate may be better at different stages.
Here’s the study on chocolate(along with other calcium enriched foods) consumption in girls:
“High calcium intake during childhood has been suggested to increase bone mass accrual, potentially resulting in a greater peak bone mass. Whether the effects of calcium supplementation on bone mass accrual vary from one skeletal region to another, and to what extent the level of spontaneous calcium intake may affect the magnitude of the response has, however, not yet been clearly established. In a double-blind, placebo–controlled study, 149 healthy prepubertal girls aged 7.9+/-0.1 yr (mean+/-SEM) were either allocated two food products containing 850 mg of calcium (Ca-suppl.) or not (placebo) on a daily basis for 1 yr. Areal bone mineral density (BMD), bone mineral content (BMC), and bone size were determined at six sites by dual-energy x-ray absorptiometry. The difference in BMD gain between calcium-supplemented (Ca-suppl.) and placebo was greater at radial (metaphysis and diaphysis) and femoral (neck, trochanter, and diaphyses) sites (7-12 mg/cm2 per yr) than in the lumbar spine (2 mg/cm2 per yr). The difference in BMD gains between Ca-suppl. and placebo was greatest in girls with a spontaneous calcium intake below the median of 880 mg/d. The increase in mean BMD of the 6 sites in the low-calcium consumers was accompanied by increased gains in mean BMC, bone size, and statural height. These results suggest a possible positive effect of calcium supplementation on skeletal growth at that age. In conclusion, calcium–enriched foods significantly increased bone mass accrual in prepubertal girls, with a preferential effect in the appendicular skeleton, and greater benefit at lower spontaneous calcium intake.”
“Both statural height and body weight, however, were significantly greater among the spontaneously high- versus low-calcium consumers (129.160.7 vs. 126.560.7 cm, P , 0.001; 27.560.5 vs. 25.760.5 kg, P , 0.001, respectively). ”
There were several non calcium enriched foods in the study and not just chocolate so it’s likely the calcium and not the chocolate making the girls taller.