Unfortunately, as of now there is no clear direction on how to manipulate the circadian clock to alter longitudinal bone growth.
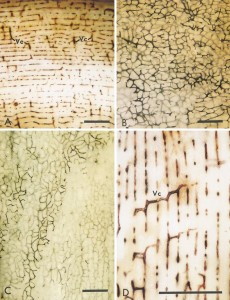
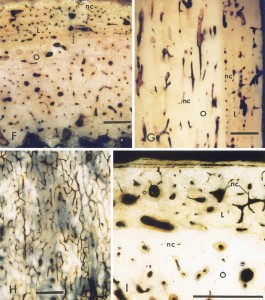
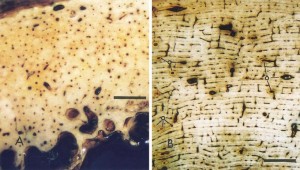
“we revealed a robust and extremely long-lasting circadian rhythm in ex vivo culture maintained for over six months from the femoral bone of a PERIOD2(Luciferase) mouse{How do we manipulate or re-initiate this circadian cycle for height growth?}. Furthermore, we also identified robust circadian clocks in flat bones. High- or low-magnification real-time bioluminescence microscopic imaging revealed that the robust circadian rhythms emanated from the articular cartilage and the epiphyseal cartilage within the growth plate of juvenile animals. Stimulation by forskolin or dexamethasone treatment caused type 0 phase resetting, indicating canonical entraining properties of the bone clock. Together, our findings from long-term ex vivo culture revealed that “tissue-autonomous” circadian rhythm in the articular cartilage and the growth plate of femoral bone functions for several months even in an organ culture condition, and provided a useful in vitro assay system investigating the role of the biological clock in bone formation or development.”
“the plasma PTH rhythm persisted under “constant routine” conditions where subjects were deprived of any exogenous time information, indicating that the rhythm is driven by the intrinsic circadian clock”
“At the molecular level, the circadian clock is composed of a set of clock genes forming cell-autonomous transcription/translation feedback loops; the molecular oscillators in turn drive the expression of output genes governing a variety of clock-controlled physiological processes. Specifically, two transcription factors, BMAL1 and CLOCK, heterodimerize and transactivate core clock genes such as Period genes (Per1 and Per2), Cryptochome1 (Cry1), and Rev-Erb genes (Rev-Erbα and Rev-Erbβ). Expressions of these genes (Bmal1, Per1, Per2, Cry1, Cry2, RevErbα and RevErbβ) show clear circadian rhythms with distinct peak times”
“circadian bioluminescence rhythms from long bones (proximal femoral ends and radiuses) and flat bones (calvariae and scapulae) showed similar period lengths”<-so the circadian rhythm may not be something that distinguishes between long and flat bones.
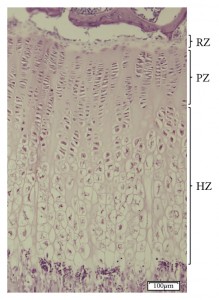
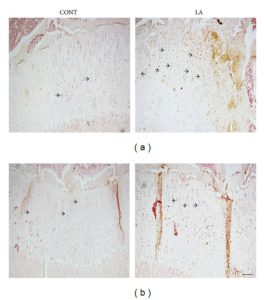
“both epiphyseal cartilage and articular cartilage in femoral trochlea showed clear circadian rhythms for 4 days”
“expression of certain clock genes has been shown in growth plates”
” local circadian clocks in the epiphyseal cartilage may affect bone growth in juvenile animals.”
“Exogenous time cues (e.g. light) can reset internal clocks.”
“[The] phase of the bone clock [that] was strongly altered by forskolin, functions to increase intracellular cAMP levels through adenylate cyclase activation. Therefore, it is possible that in vivo circadian phase can be reset by endogenous substance(s) via the cAMP pathway in the bone. The hormone PTH increases intracellular cAMP levels via the PTH/PTHrP receptor, consequently inducing Per1 and Per2 expression through the cAMP–PKA–CREB pathway. In addition, sympathetic signaling stimulated by leptin has been shown to regulate bone remodeling in part through a β-adrenergic receptor (β-AR). The β-AR agonist isoproterenol also enhances intracellular cAMP levels and up-regulates Per1/2 and Bmal1 expression in primary mouse osteoblasts. In accordance, isoproterenol has been reported to stimulate the circadian rhythmic expression of Per1/2/3 and Bmal1 in human SaM-1 osteoblastic cells”
“DEX, synthetic glucocorticoids (GCs), was found to reset the bone circadian rhythm. GCs are secreted from the adrenal gland in a circadian manner. Although the SCN is not reset by GCs due to a lack of glucocorticoid receptor (GR) expression, circadian clocks in peripheral organs such as the liver, kidney, and heart are highly responsive to GCs. GCs are considered as internal time-cues which relay timing information within the body and synchronize the peripheral clocks, including bones, as shown here. At the molecular level, GCs bind to GR and regulate target gene expression via glucocorticoid response elements. Previous studies have identified Per1, Per2, and E4bp4 as direct targets of GRs in mice”
Forskolin alters Ca2+ and cAMP levels, I haven’t seen any studies regarding the effects of Forskolin on longitudinal bone growth. Dexamethasone is widely known to inhibit longitudinal bone growth. However, Dexamethasone is also known to help induce chondrogenic differentiation.