I’m still working on height increase. Just doing more independent research and learning more about anatomy and physiology and actions of cells as the research I’m looking at is a lot of the same old, same old. Maybe the key is to look at older studies before things were set in their ways. It seems in the old days they were willing to try new risks to get people to grow taller.
Essentially the study found that heat did not increase bone length however there was some promise in that decalcification could be caused by the heat and that could enable longitudinal bone growth. And the study shows islands of cartilage which could be the creation of new growth plates which is quite promising. But the heat itself actually didn’t stimulate the growth plate itself. It was only the heat degeneration the calcified bone matrix and stimulating the creation of growth plate islands that incurred new growth.
The effect of heat upon the growth of bone
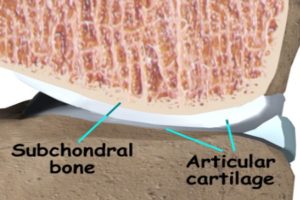
“GROWTH in length of long bones consists of two mutually independent processes, the division and palisade arrangement of cartilage cells, and the subsequent calcification of the matrix between these cells and its replacement by bone. It is generally agreed that growth is dominated by the activities of the cells of the reserve zone and those in the adjacent apex of the cartilage columns. The subsequent enmeshment, of hypertrophic cartilage cells within a calcified matrix must prevent elongation at other sites. Recent attempts to stimulate the growth of bone have been based upon the production of an irritative lesion within the metaphysis, stimulating ossification rather than cartilage-cell division. ”
“Chapchal and Zeltienrust (1947-48) reported an inconstant increase in the rate OF growth in the rabbit after the insertion of metal or ivory pins within the metaphysis. Wilson (1952) using copper and constantan wire in the dog produced similar results. The application of these methods to limb inequality in children has been reported by Pease (1962). Metal or ivory screws WPI’P inserted transversely into the metaphysis of the femur and tibia. Each of the seven children subjected to this procedure showed an increase in the rate of growth of the shorter limb, but equalization of length was not attained. ”
“The overgrowth of bone which is constantly seen after fractures, in the presence of arteriovenous aneurysms, and in association with bone and joint infections”
arteriovenous aneurysm an abnormal communication between an artery and a vein in which the blood flows directly into a neighboring vein or is carried into the vein by a connecting sac.<-Lateral loading can increase blood flow. Though this probably won’t work without existing growth plates.
“increase in the length of a limb following the production of an arteriovenous fistula in the dog”
“One of the clinical features of most cases of limb elongation with an increase in the temperature of the skin, and in the arteriovenous aneurysm this is associated with an increase in the temperature of bone”
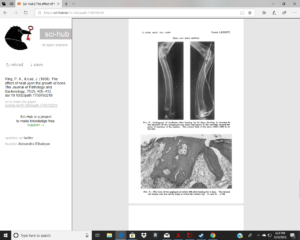
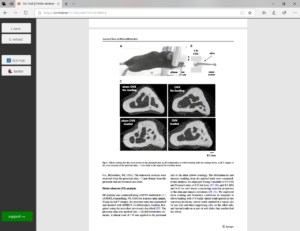
“The rate of growth of the ulna was in some animals slightly depressed, in rabbit 480 markedly SO. In this animal there was considerable formation of new bone around tJie resistor, although the epiphyseal cartilage appeared normal. The overgrowth of the ulna noted in rabbit 465 was not associated with any abnormal histological appearance of the epiphyseal cartilage and the radiographs suggest that the discrepancy may have been due to a disturbance of growth in the control limb. The radiographs also show a relative decalcification of the the whole of the treated forelimb and this may have been associated with a generalized hyperemia{excess of blood in the vessels} of this limb.”
“Where the heating level was high, the epiphyseal cartilage is affected. The earliest changes in this region are an irregularity of the cartilage columns and a granularity of the matrix. When cellular destruction occurs it is at first confined to the region of the apex of the cartilage columns and is associated with fibrillation of the cartilage matrix. ”
“In only one animal (465) did an increase in bone length occur. This animal was heated for two days and, the wires having broken, the resistor was left unheated for a further 36 days. Although the increase in length of the limb was considerable, aid was associated with a generalized decalcification of the forelimb, suggesting an increase in the vascularity of this member, the difference in length of the limbs may have been due to some abnormality of growth on the control side. “<-So decalcification is key to growing taller. High levels of heat can was found to cause necrosis which reduced growth but if decalcification can enhance growth. Then maybe heat could enhance growth by decalcifying bones.
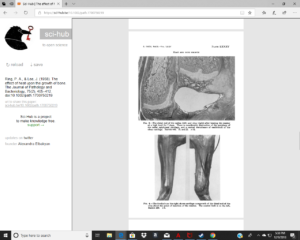
“heat has been shown to stimulate the production of cartilage around the resistor and to produce islands of endochondral ossification within the bony epiphysis and along the shaft of the radius.”<-islands of endochondral ossification is promising because it shows new induction of bone growth.
“Islands of cartilage were produced within the bony epiphysis close to the resistor, and along the ulnar border of the radial shaft. Some of them islands showed endochondral ossification, but there was no increase of cellular activity in the epiphyseal cartilage. A large cartilaginous mass developed in the region where the resistor was buried, and, in many animals, the transverse diameter of the metaphysis was greatly increased. ”
Figure 8 is an image near the resistor so there should be islands of cartilage visible. I can’t tell If there are cartilage islands or not and if there are cartilage islands we can’t say for sure whether they are not just broken off cartilage from the growth plate. Cartilage islands within the diaphysis would be key to seeing if heat can induce new growth plates.
Here’s mentioned overgrowth.