This is going to be one of those posts which will definitely change the direction and content of this website. It is game changing, since it shows that we are getting much, much closer than before. Much closer than I expected, which is a shock to me. I am just amazed at just how close we just might be. Its seems like all the technical difficulties in theory has almost all been removed. Now, I feel like all that is standing in our way is funding, to get this laboratory success to be taken into the public/real world and applied.
This is going to be one of those posts which will definitely change the direction and content of this website. It is game changing, since it shows that we are getting much, much closer than before. Much closer than I expected, which is a shock to me. I am just amazed at just how close we just might be. Its seems like all the technical difficulties in theory has almost all been removed. Now, I feel like all that is standing in our way is funding, to get this laboratory success to be taken into the public/real world and applied.
Just 10 minutes ago I found out that one of the primary researchers I have been tracking, Professor Eben Alsberg, has been working on the exact, the EXACT same type of research that I have been proposing we should be working on.
Not only that, I barely missed meeting Dr. Alsberg. Apparently he was one of the speakers that was attending the 2015 World Termis Conference on Regenerative Medicine in Boston back in August. I was in Boston at the exact same time, at the sister conference of Termis, the Organ-On-A-Chip one. Apparently the Termis Conference was going on at the exact same days (off by 1 day) and around the exact same Boston area. Alsberg was in attendence maybe just 1000 feet away from me. Many of the people who went to the conference I went to, like the company representatives of Cellink (from Sweden), were going to the Termis Conference as well. At the time, I thought that it would only be Dr Atala of Wake Forest who would be there, and no one really close to doing the type of research I was hoping for. Well, I was wrong, extremely wrong.
Originally, I found out about Dr. Alsberg from a reader of the website who sent me a link to Alsberg’s paper on creating the first evidence of functional growth plates. Well, it turns out that for more than a decade (maybe 14 years after) after that 2001 paper came out, Alsberg and his team of researchers based in Case Western University has been fine-tuning the cartilage regeneration technique.
I would like the readers to refer to 6 sources I would like to use to validate my idea that Alsberg, like maybe 4-5 main other researchers, is working on something really close to our holy grail. I thought that no one was attacking the problem that we wanted to be solved. I was wrong again.
Alsberg is trying to regeneration the growth plate, and not just in 1 single approach. He is trying ideas which I thought was pure science fiction, the type you see in comic books.
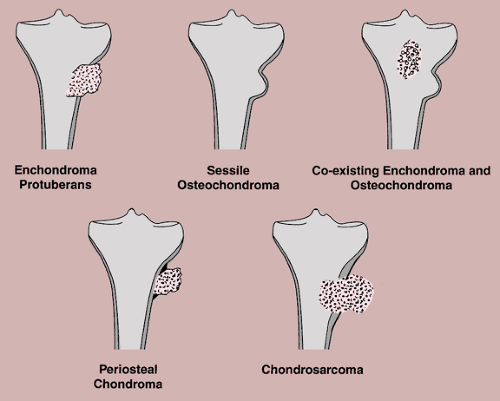
Tyler and I have both agreed that the only way one could possibly “reopen” the growth plates is if a tissue engineering type biomedical engineer could solve the problem of converting bone tissue to cartilage tissue, which is basically one of many types of cell-to-cell transformation, known by the scientific term Transdifferentiation.{Tyler-also you could create miniature breaks in the bone and induce stem cell differentiation into cartilage; but some growth plate cells may transdifferentiate into osteoblasts and may maintain the growth plate cartilage genetic material so by converting them back to chondrocytes may be a way to create new growth plates; however, bone still places a constraint on growth so you have to find a way to weaken or break it some how}
I have said at least twice that I don’t think it was possible to figure out transdifferentiation of bone tissue into cartilage tissue, at least this century. Even for the possibility that it would ever be possible, I was pessimistic. Well, it seems that Alsberg is trying to do just that. Since he has been working on this problem far longer and more in depth than me, he would be more aware of the exact technical details in getting this type of cell transformation to work out. If he is still trying to do it, it means that he honestly believes that it is possible. Given what I already know of Alsberg, I put my faith in his ability.
Now I refer to the reader who is somewhat knowledgeable on basic biology to read over the sources I provided below.
From the sources, I have been able to make multiple conclusion, all of them extremely positive, for our endeavor.
1. Alsberg is researching how to convert bone to cartilage. If he succeeds, which he believes is just a cell spatial-gradient and signaling issue, then we can create cartilage in the middle of bone tissue. This is a non-invasive way of growing taller!!{Tyler-Note that LSJL involves a pressure gradient and affects cell signaling}
2. Alsberg is researching how to implant cartilage (lab grown/in-vitro) back into the body.
3. Alsberg is researching how to grow cartilage tissue in the lab to be strong enough to handle the en vivo environment.
4. Alsberg already succeeded in growing growth plates almost 15 years ago, from a paper he wrote in 2001.
5. Alsberg believes that the trick to get the lab-grown osteo-chondrogenic tissue to expand is to get the spatial gradient of the cells inside the ECM to be in a certain orientation. So he already has figured that out.{Tyler-Interesting, maybe we can alter the spatial gradient within the bone via mechanical means}
6. If you look at the papers he has published from source 6 that I provided below, you can see that his research is basically circling around and around the research that is our holy grail. I did not believe that he would actually be doing the exact type of research we are hoping for, but he is. Technically, he never actually wrote that he is trying to grown functional growth plates to be reimplanted back in the body, but the 5 first sources reveal enough. A simple reader would be able to put the pieces together to form the overall picture. Alsberg is trying to to get growth plates to work out.
This type of research I did not expect for another 10 years., at least not someone who is actively tackling the exact problem. I suspect that probably by the year 2020, Alsberg with Ballock will have written a paper discussing the viability and possibility of implanting their lab grown physeal-like tissue into bone defects (from osteonomy) to increase the length of bone for people who are past the stage of bone maturity. If they believe that there is a financial windfall from taking their research into market, (aka a rich saudi prince funds them a 9-figure check to get the stuff from of lab-to public), the world will be changing in a dramatic way.
In another 15 years maybe, if they get the signaling correct, they might come out with a 2nd different way of making bones longer, by using transdifferentiation. If they are successful in doing that, we will have reached out holy grail. Imagine our grandchildren always having a non-invasive technique to make their bones longer. This is right out of a science fiction book.
I promise the readers that I will go into more detail in a 2nd post, going deeper on the science, and also creating a picture of what is possible, if Alsberg with Ballock are successful. From the looks of it, they are going to succeed, and it might not just be them. There seems to be at least another team that I am aware of, which are working on something very similar to them.
It might turn out that within 15-20 years, there will be more than 1 company who are racing towards getting this limb lengthening surgery alternative out into the market for the general public to use. As for the trandifferentiation possibility, that probably won’t come about for another 50 years at least, after I am gone. When that happens, I will be happy that finally the short statured people around the world can finally let out a breathe of relief.
Note: Of course, there is indeed a limit to how much we can length the bones of a person. Making a person who is 5 ft to 6 ft is technically possibly, but the result may be slightly weird. Not only that, what if an already tall person wants to go through with this treatment, turning themselves into 8 feet??
—————————————————————————————————————-
Refer to source #1 – http://www.news-medical.net/news/20130919/Innovative-system-can-help-manipulate-stem-cells-to-repair-damaged-tissues-and-organs.aspx
Scientists know that physical and biochemical signals can guide cells to make, for example, muscle, blood vessels or bone. But the exact recipes to produce the desired tissues have proved elusive.
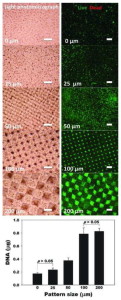
Now, researchers at Case Western Reserve University have taken a step toward identifying that mix by developing an easy and versatile way of forming physical and biochemical gradients in three dimensions.
Ultimately, one of their goals is to engineer systems to manipulate stem cells to repair or replace damaged tissues and organs.
“If we can control the spatial presentation of signals, we may be able to have more control over cell behavior and enhance the rate and quality of tissue formation,” said Eben Alsberg, an associate professor of biomedical engineering and orthopaedic surgery at Case Western Reserve and senior author of the research. “Many tissues form during development and healing processes at least in part due to gradients of signals: gradients of growth factors, gradients of physical triggers.”
Alsberg, postdoctoral scholar Oju Jeon and graduate student Daniel S. Alt of Case Western Reserve, and Stephen W. Linderman, a visiting undergraduate on a National Science Foundation Research Experience for Undergraduates summer fellowship, tested their system on mesenchymal stem cells, turning them toward bone or cartilage cells. They report their findings in Advanced Materials.
Regulating the presentation of certain signals in three-dimensional space may be a key to engineering complex tissues, such as repairing osteochondral defects, damaged cartilage and bone in osteoarthritic joints, Alsberg said.
“There must be a transition from bone to cartilage,” he said, “and that may require control over multiple signals to induce the stem cells to change into the different kinds of cells to form tissues where you need them.”
In their first test, the researchers found that stem cells changed into cartilage or bone cells in the directions of two opposing soluble growth factor gradients: one that promotes cartilage, called TGF-beta 1, and another that promotes bone, called BMP-2{Tyler-Interesting that BMP-2 has been used to promote cartilage in tissue engineering as well}. The stem cells were placed in a solution of modified alginate, a material derived from seaweed that can form a jello-like material called a hydrogel when exposed to low level ultraviolet light.
The solution was divided between two computer-controlled syringe pumps, with BMP-2 in one syringe and TGF-beta 1 in the other. By controlling the rate of injection with the pumps and using a mixing unit, a hydrogel with a BMP-2 gradient starting with a large amount and tapering to nearly none and an opposing TGF-beta 1 gradient from low-to-high was formed.
The hydrogels were further modified in such a way that the growth factors were retained for a longer period of time. This enabled prolonged exposure of stem cells to the growth factors and further control over their differentiation into bone or cartilage cells.
The researchers then modified the hydrogel with a gradient of adhesion ligands, molecular strings that allow the stem cells to attach to the hydrogel itself. After two weeks of culturing the cells, they found the highest number of cells in the hydrogel region where the concentration of ligands was highest.
In a third test, they created a gradient of crosslink density within the hydrogels. Crosslinks provide structure to the gels. The lower the density, the more flexible the hydrogel; the higher, the stiffer the gel.
After two weeks, more cells were found in the most flexible gel regions within the gradient. The flexibility may allow for more free movement of nutrients and removal of waste products, Alsberg explained.
“This is exciting,” Alsberg said. “We can look at this work as a proof of principle. Using this approach, you can use any growth factor or any adhesion ligand that influences cell behavior and study the role of gradient presentation. We can also examine multiple different parameters in one system to investigate the role of these gradients in combination on cell behavior.”
If the technology enables them to unravel recipes that generate complex tissues, the biodegradable hydrogel mix could be implanted or injected at the site of an injury, the researchers say. The recipe would guide cell behavior until new tissue is formed, restoring function.
Refer to Source #2: Environmental cues to guide stem cell fate decision for tissue engineering applications
Abstract: The human body contains a variety of stem cells capable of both repeated self-renewal and production of specialised, differentiated progeny. Critical to the implementation of these cells in tissue engineering strategies is a thorough understanding of which external signals in the stem cell microenvironment provide cues to control their fate decision in terms of proliferation or differentiation into a desired, specific phenotype. These signals must then be incorporated into tissue regeneration approaches for regulated exposure to stem cells. The precise spatial and temporal presentation of factors directing stem cell behaviour is extremely important during embryogenesis, development and natural healing events, and it is possible that this level of control will be vital to the success of many regenerative therapies. This review covers existing tissue engineering approaches to guide the differentiation of three disparate stem cell populations: mesenchymal, neural and endothelial. These progenitor cells will be of central importance in many future connective, neural and vascular tissue regeneration technologies.
Refer to Source #3: http://www.termis.org/wc2015/docs/programWednesday.pdf
Refer to Source #4: New Method Grows Thicker, Stiffer Cartilage
Many research labs are busy working away at developing better tissue engineering techniques to grow replacement parts for aged and damaged human bodies. Here’s a lab at Case Western that has developed a new and promising cartilage growth technique.
A lab discovery is a step toward implantable replacement cartilage, holding promise for knees, shoulders, ears and noses damaged by osteoarthritis, sports injuries and accidents.
Self-assembling sheets of mesenchymal stem cells permeated with tiny beads filled with growth factor formed thicker, stiffer cartilage than previous tissue engineering methods, researchers at Case Western Reserve University have found. A description of the research is published in the Journal of Controlled Release.
“We think that the capacity to drive cartilage formation using the patient’s own stem cells and the potential to use this approach without lengthy culture time prior to implantation makes this technology attractive,” said Eben Alsberg, associate professor in the departments of Biomedical Engineering and Orthopaedic Surgery, and senior author of the paper.
Think of all the people with painful knees, fingers, and other joints because their cartilage has worn down. The ability to fix all these damaged joints would cut pain and increase mobility. Increased mobility would also increase exercise and muscle mass.
Among successful tissue engineering projects so far: functional replacement mouse pituitary glands, replacement urethras for kids, and bladders for adults. The list is going to grow every year and the rate of growth is going to accelerate.
By Randall Parker 2011 December 04 09:57 PM
A lab discovery is a step toward implantable replacement cartilage, holding promise for knees, shoulders, ears and noses damaged by osteoarthritis, sports injuries and accidents.
Self-assembling sheets of mesenchymal stem cells permeated with tiny beads filled with growth factor formed thicker, stiffer cartilage than previous tissue engineering methods, researchers at Case Western Reserve University have found. A description of the research is published in the Journal of Controlled Release.
“We think that the capacity to drive cartilage formation using the patient’s own stem cells and the potential to use this approach without lengthy culture time prior to implantation makes this technology attractive,” said Eben Alsberg, associate professor in the departments of Biomedical Engineering and Orthopaedic Surgery, and senior author of the paper.
Alsberg teamed with biomedical engineering graduate students Loran D. Solorio and Phuong N. Dang, undergraduate student Chirag D. Dhami, and Eran L. Vieregge, a student at Case Western Reserve School of Medicine.
The team put transforming growth factor beta-1 in biodegradable gelatin microspheres distributed throughout the sheet of stem cells rather than soak the sheet in growth factor.
The process showed a host of advantages, Alsberg said.
The microspheres provide structure, similar to scaffolds, creating space between cells that is maintained after the beads degrade. The spacing results in better water retention – a key to resiliency.
The gelatin beads degrade at a controllable rate due to exposure to chemicals released by the cells. As the beads degrade, growth factor is released to cells at the interior and exterior of the sheet, providing more uniform cell differentiation into neocartilage.
The rate of microsphere degradation and, therefore, cell differentiation, can be tailored by the degree to which the microsphere are cross-linked. Within the microspheres, the polymer is connected by a varying number of threads. The more of these connections, or cross-links, the longer it takes for enzymes the cell secretes to enter and break down the material.
The researchers made five kinds of sheets. Those filled with: sparsely cross-linked microspheres containing growth factor, highly cross-linked microspheres containing growth factor, sparsely cross-linked microspheres with no growth factor, highly cross-linked microspheres with no growth factor, and a control with no microspheres. The last three were grown in baths containing growth factor.
After three weeks in a petri dish, all sheets containing microspheres were thicker and more resilient than the control sheet. The sheet with sparsely crosslinked microspheres grew into the thickest and most resilient neocartilage.
The results indicate that the sparsely cross-linked microspheres, which degraded more rapidly by cell-secreted enzymes, provided a continuous supply of growth factor throughout the sheets that enhanced the uniformity, extent, and rate of stem cell differentiation into cartilage cells, or chondrocytes.
The tissue appeared grossly similar to articular cartilage, the tough cartilage found in the knee: rounded cells surrounded by large amounts of a matrix containing glycosaminoglycans. Called GAG for short, the carbohydrate locks water ions in the tissue, which makes the tissue pressure-resistant.
Testing also showed that this sheet had the highest amount of type II collagen – the main protein component of articular cartilage.
Although the sheet was significantly stiffer than control sheets, the mechanics still fell short of native cartilage. Alsberg’s team is now working on a variety of ways to optimize the process and make replacement cartilage tough enough for the wear and tear of daily life.
One major advantage of this system is that it may avoid the troubles and expense of growing the cartilage fully in the lab over a long period of time, and instead permit implantation of a cartilage sheet into a patient more rapidly.
Because the sheets containing microspheres are strong enough to be handled early during culturing, the researchers believe sheets just a week or two old could be used clinically. The mechanical environment within the body could further enhance cartilage formation and increase strength and resiliency of the tissue, completing maturation.
Refer to Source #6: http://www.aptcenter.research.va.gov/pdfs/cvs/Alsberg-Eben-CV.pdf