This paper provides some support that mechanical loading stimulates the fluid contents of the bone(angiogenesis is the formation of new blood vesses). Lateral impact loading is the what I view as the most direct and effective method to move the fluid contents within the bone.
This paper is also by both Yokota and Zhang. Papers such as those below strongly support the use of lateral impact loading for bone tissue stimuli. That lateral impact loading will increase height requires additional leaps.
Before that paper here’s some information about Type H blood vessels.
Motivating role of type H vessels in bone regeneration
“Coupling between angiogenesis and osteogenesis has an important role in both normal bone injury repair and successful application of tissue‐engineered bone for bone defect repair. Type H blood vessels are specialized microvascular components that are closely related to the speed of bone healing. Interactions between type H endothelial cells and osteoblasts, and high expression of CD31 and EMCN render the environment surrounding these blood vessels rich in factors conducive to osteogenesis and promote the coupling of angiogenesis and osteogenesis. Type H vessels are mainly distributed in the metaphysis of bone and densely surrounded by Runx2+ and Osterix+ osteoprogenitors{Hence why we may want to tap the metaphysis}. Several other factors, including hypoxia‐inducible factor‐1α, Notch, platelet‐derived growth factor type BB, and slit guidance ligand 3 are involved in the coupling of type H vessel formation and osteogenesis. In this review, we summarize the identification and distribution of type H vessels and describe the mechanism for type H vessel‐mediated modulation of osteogenesis. Type H vessels provide new insights for detection of the molecular and cellular mechanisms that underlie the crosstalk between angiogenesis and osteogenesis. As a result, more feasible therapeutic approaches for treatment of bone defects by targeting type H vessels may be applied in the future.”
” use of the immunosuppressive drug rapamycin, which has anti‐angiogenic properties, inhibited neovascularization in the fracture callus and delayed fracture healing.”
“Vessels can not only maintain the high metabolic demand for nutrients and oxygen in the callus, but also provide pathways for cells such as inflammatory cells, fibroblasts and osteoblast/osteoclast precursors to enter the defect area.”
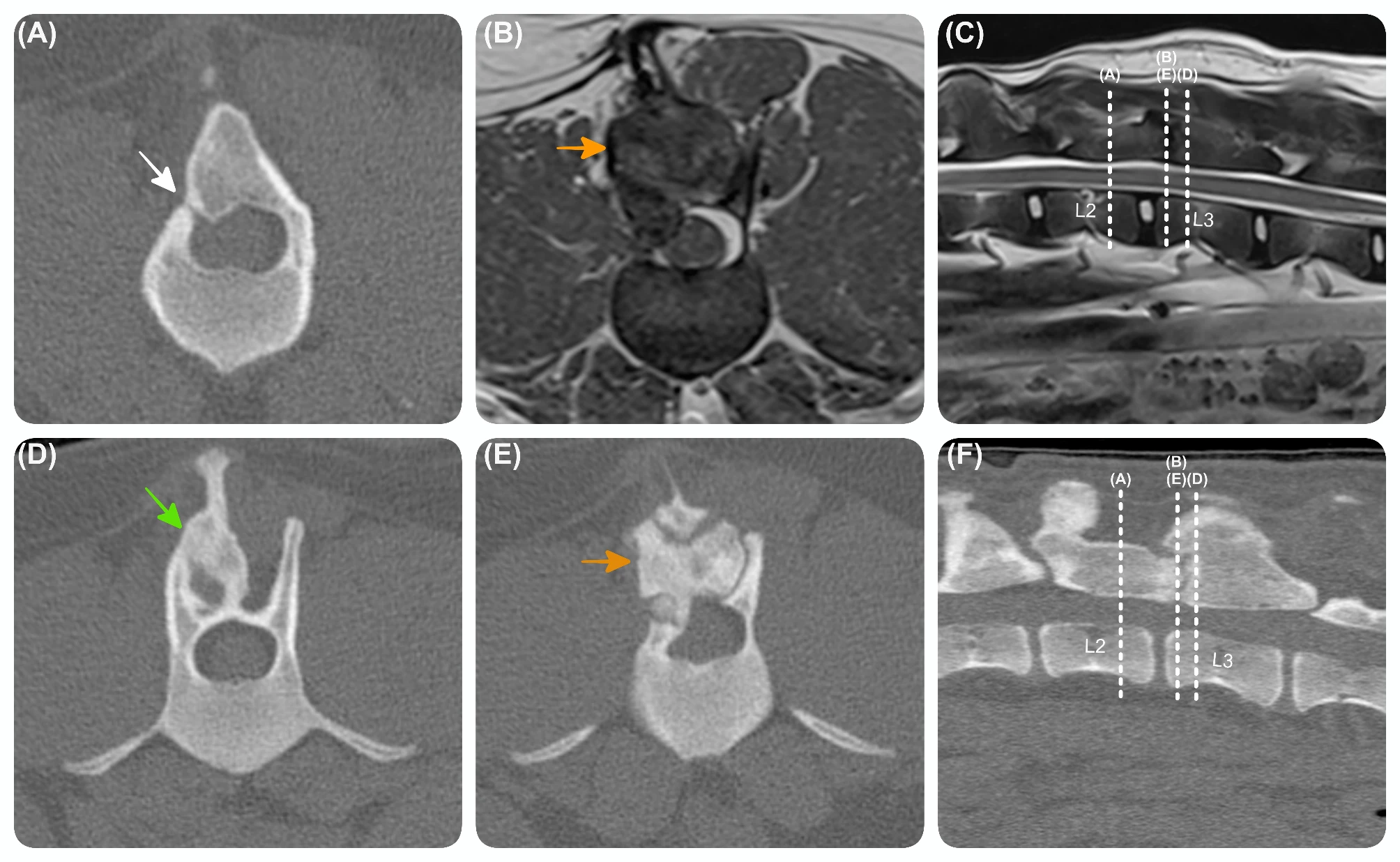
“There are two subtypes of vessels, type H vessels and type L vessels, in the capillaries of the metaphysis and bone marrow cavity. These vessels are classified according to their specialized ECs that have specific molecular and morphological properties. Type H vessels are mainly distributed in the metaphyseal region and sub‐periosteum and show strong positive staining with antibodies against two kinds of EC proteins (CD31 and EMCN), while type L vessels are mainly distributed in the diaphyseal region and show weak positive staining for CD31 or EMCN. Type H vessels are interconnected by distal vessel loops or arches and resemble straight columns, while type L vessels mainly located in the diaphysis display a highly branched pattern characteristic of the sinusoidal vasculature of the bone marrow. These two types of vessels are closely connected at the epiphysis‐diaphysis junction and form a complete vascular bed in the bone marrow cavity”
“Although type H ECs only account for 1.77% of all bone ECs and 0.015% of total bone marrow ECs, a large number of bone progenitor cells, which can differentiate into osteoblasts and osteocytes, are distributed around these vessels, suggesting that type H vessels may be a potent promoter of bone regeneration. The dense distribution of Runx2+ osteoprogenitors and osteoblasts around these CD31+ vessels in the metaphysis and endosteum confirms their role as a potent promoter of bone regeneration. In contrast, type L vessels have almost no surrounding bone progenitor cells. The two types of ECs were isolated and purified from bone tissue and evaluated for their levels of mRNA expression for secreted growth factors that promote the survival and proliferation of bone progenitor cells. The transcript levels for Pdgfa, Pdgfb, Tgbf1, Tgfb3 and Fgf1 in type H ECs were significantly higher than those in type L ECs. These secretory growth factors are closely related to the proliferation and survival of bone progenitor cells Thus, the findings further confirm a key role for type H vessels in bone regeneration. Type H vessels can transit to type L vessels, suggesting that type H ECs may be the upstream ECs in bone.”<-this may suggest that tapping the epiphysis would be more effective to gaining height as it transmits the bone progenitor cells from the epiphysis to diaphysis. But I did not gain any height for years by tapping the epiphysis. The only period where I showed potential height was where I tried tapping the diaphysis. I believe this may be due to fused growth plates blocking effective movement between the epiphysis and diaphysis. This blockage is somewhat shown by the fact that while the epiphysis houses red bone marrow the diaphysis the yellow bone marrow which you wouldn’t expect unless there was some sort of bloackage. However, the metaphysis holds these type H vessels which I recommend tapping there.
“The proliferation ability of type H vascular ECs in young individuals was significantly stronger than that in adult individuals, while the proliferation ability of type L vascular ECs did not differ significantly between young and old individuals.”
“Notch signalling in type H vascular ECs plays a key role in mediating vascular formation and osteogenic coupling. Cell proliferation and high expression of Noggin protein occur in type H vascular ECs under the action of Notch signalling. Noggin protein can promote proliferation and differentiation of osteoblastic progenitor cells as well as maturation and hypertrophy of chondrocytes. Mature and hypertrophic chondrocytes can guide vascular budding through high secretion of VEGF and promote the generation of new blood vessels. Through the combination of Notch signalling by ECs, Noggin and VEGF, the processes of osteogenesis and angiogenesis are linked together. After blockade of Notch signalling in ECs, vessel disorganization, cartilage defects, reduced bone trabeculae and many other low osteogenesis manifestations were found in bone marrow. These results indicate that type H vessels play important roles in mediating growth of blood vessels, maintaining number of perivascular bone progenitor cells and coupling of osteogenesis and angiogenesis”
“MMP‐9 released from type H ECs, not osteoclasts, are essential for resorbing cartilage to lead longitudinal bone growth”
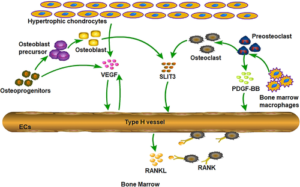
“When the expression level of PDGF‐BB was knocked down in adult mice, the number of type H vessels was significantly decreased, accompanied by reductions in trabecular bone and cortical bone mass.”
“When a bone defect occurs, monocyte/macrophage lineage cells such as tartrate‐resistant acid phosphatase‐positive (TRAP+) mononuclear cells and osteoblastic cells move to the bone defect area and secrete PDGF‐BB to recruit PDCs for osteogenesis.”
“low‐intensity pulsed ultrasound (LIPUS) can promote blood flow and angiogenesis in the fracture healing process. LIPUS induced substantial increases in osteoblast proliferation and type H vessel number in a rat spinal fusion model. The matrix modification properties of matrix metalloproteinases (MMPs) can also affect angiogenesis and bone formation.MMP‐2 promoted a marked increase in the vessel number in bone, while type H ECs released MMP‐9 with a key role in resorption of articular cartilage during growth of long bones”<-I believe Lateral Impact Loading will strongly beat LIPUS in stimulating fluid flow just by basis of the word low-intensity.
Here’s the Yokota paper:
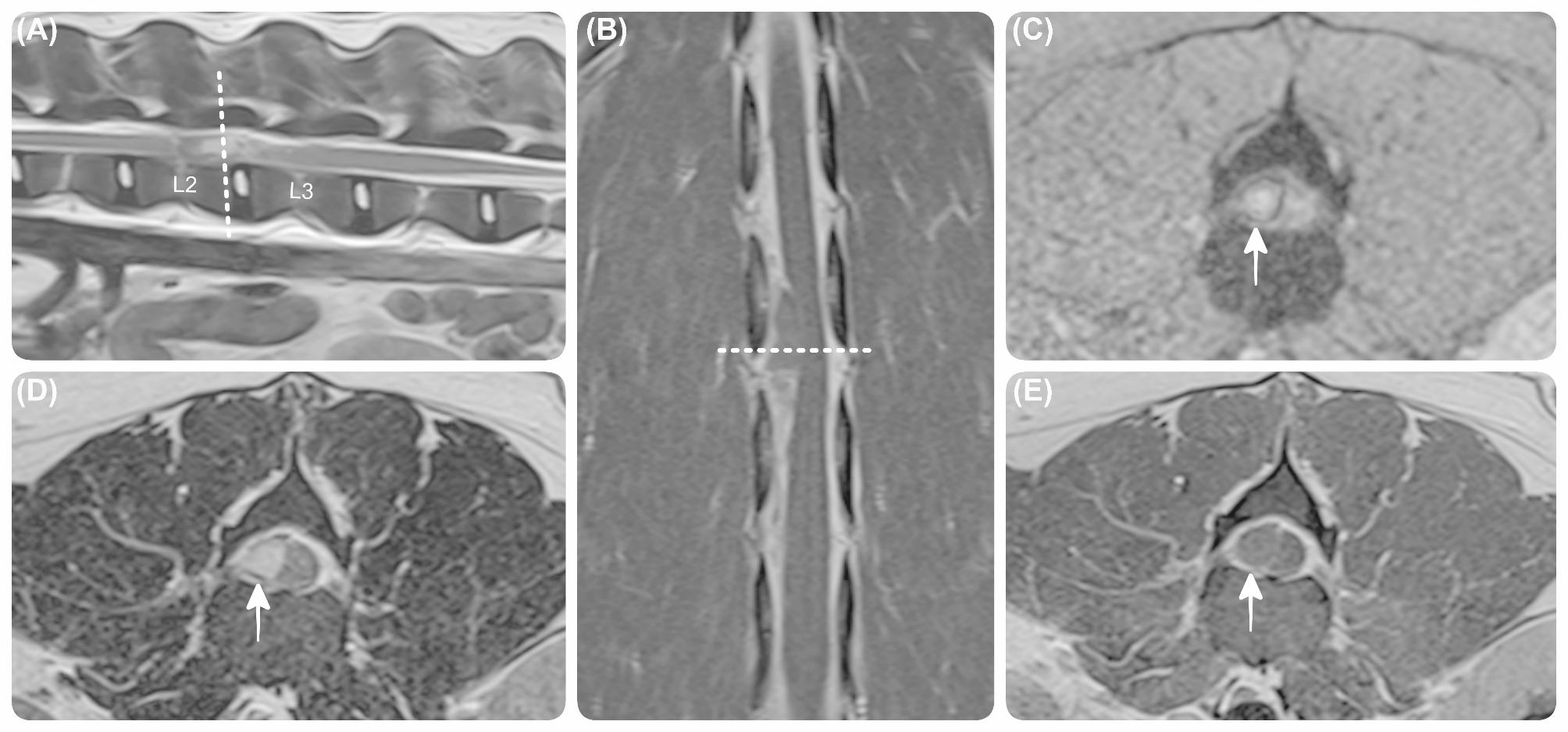
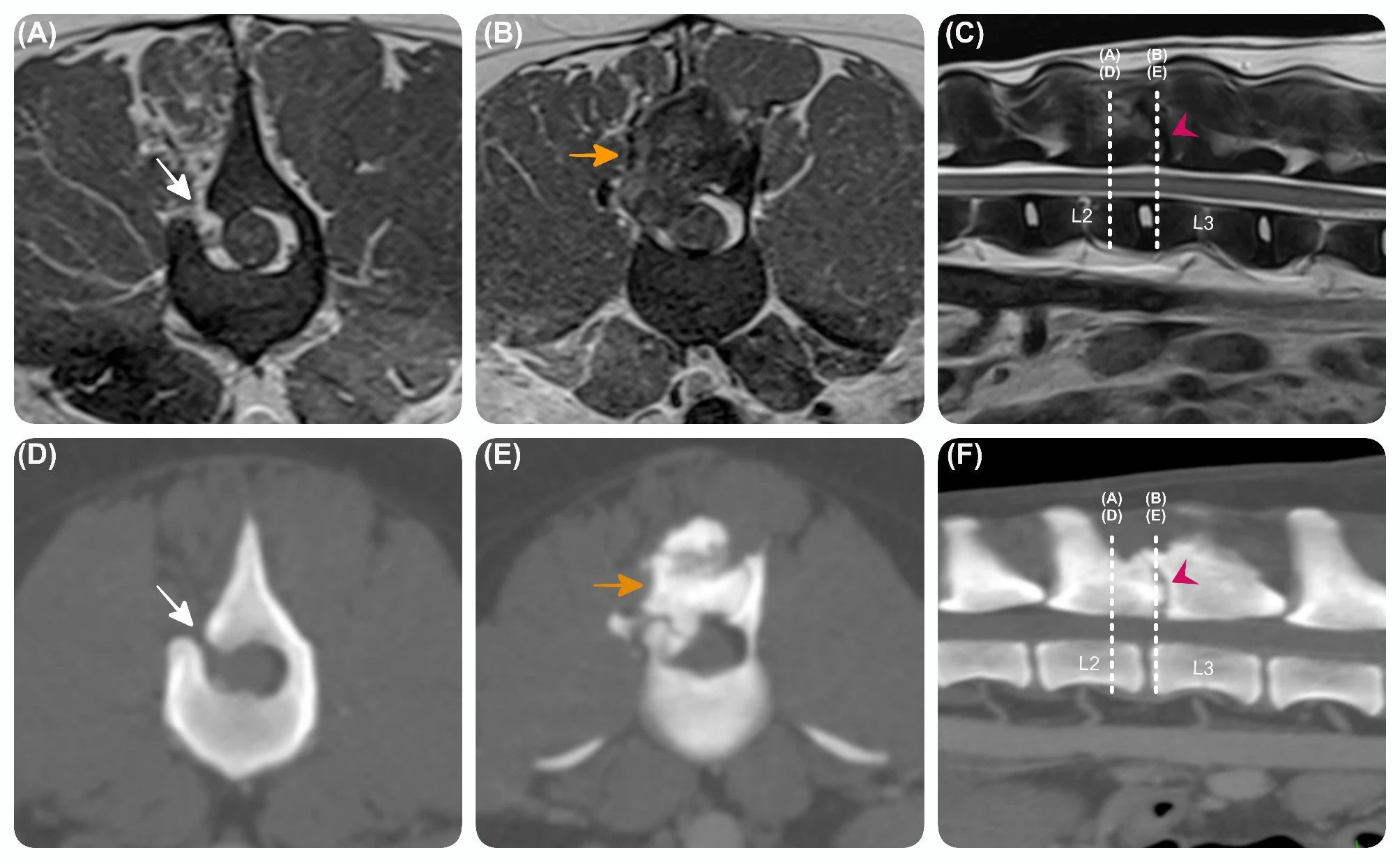
“Exosomes are important transporters of miRNAs, which play varying roles in the healing of the bone fracture. Angiogenesis is one of such critical events in bone healing, and we previously reported the stimulatory effect of mechanical loading in vessel remodeling. Focusing on type H vessels and exosomal miR‐214‐3p, this study examined the mechanism of loading‐driven angiogenesis. MiRNA sequencing and qRT‐PCR revealed that miR‐214‐3p was increased in the exosomes of the bone‐losing ovariectomized (OVX) mice, while it was significantly decreased by knee loading. Furthermore, compared to the OVX group, exosomes, derived from the loading group, promoted the angiogenesis of endothelial cells. In contrast, exosomes, which were transfected with miR‐214‐3p, decreased the angiogenic potential. Notably, knee loading{knee loading is traditional LSJL} significantly improved the microvascular volume{volume of the smallest blood vessels}, type H vessel formation, and bone mineral density and contents, as well as BV/TV, Tb.Th, Tb.N, and Tb.Sp. In cell cultures, the overexpression of miR‐214‐3p in endothelial cells reduced the tube formation and cell migration. Collectively, this study demonstrates that knee loading promotes angiogenesis by enhancing the formation of type H vessels and downregulating exosomal miR‐214‐3p.”
“In blood flow, shear stress and strain in the vessels are the major biomechanical parameters. Mechanical forces play a crucial role in vascular injury and repair, which can directly activate the mechanosensing molecules. We have developed joint loading modalities, in which dynamic lateral loads are applied to synovial joints such as the elbow, knee, and ankle.”
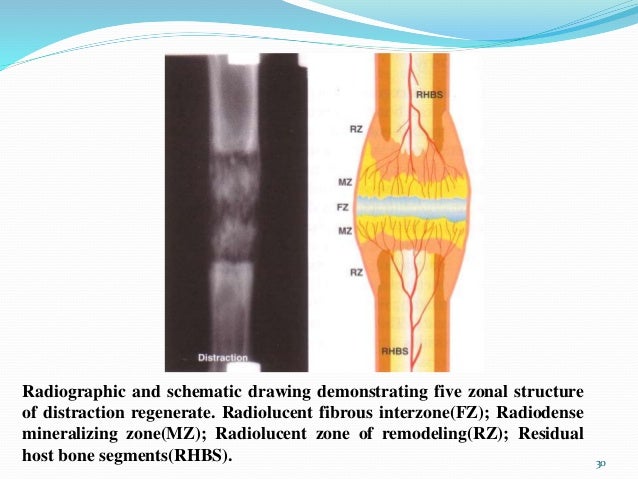
“mechanical loading induces dynamic deformation in the epiphysis that drives the alteration in intramedullary pressure in the medullary cavity and interstitial fluid flow in the lacunocanalicular network.”<-I found from experience that due to the rats not having fused growth plates this may be different than humans. The fused growth plate may reduce the the ability of the fluids from the epiphysis to reach the intermedullary cavity. It may happen somewhat but not to the extent as with open growth plates. Thus instead of targeting the epiphysis we target the metaphyseal region which is below the epiphyseal line. Also there have been studies by Yokota that have shown a limit to the bone deformation that can be achieved by lateral loading.
“knee loading stimulated wound healing in the femoral neck and tibia, prevented cartilage degeneration, and promoted vessel remodeling and bone healing in osteoporosis of the femoral head.”
“As nanometer‐scale particles, exosomes are one form of extracellular vesicles (EVs) together with microvesicles and apoptotic bodies. Exosomes are small vesicles of endocytic origin and are suggested to act as an essential mediator in intercellular communications. For instance, bone marrow‐derived mesenchymal stem cells (BMMSCs) play a vital role in osteoblastic differentiation via a paracrine pathway, and several studies have demonstrated the role of BMMSC‐derived EVs in vessel remodeling and bone healing. In vivo experiments revealed that exosomes markedly stimulated bone regeneration and angiogenesis in critical‐sized calvarial defects in ovariectomized rats”
“In the current study, loads with 1 N and 5 Hz were given for 6 min/day for 14 consecutive days.”

“compared to the sham control, OVX treatment decreased cell migration and knee loading enhanced it”

The image isn’t big enough for me to see if there’s any abnormalities.
“Mechanical forces such as shear stress and cyclic strain can regulate the adhesion, proliferation, migration, and differentiation of stem cells via serious signaling pathways. The enrichment and differentiation of stem cells play an important role in the angiogenesis and maintenance of vascular homeostasis.”
There’s no smoking gun in these studies that show that an increase in the movement of the various fluids can lead to creation of longitudinal bone growth. But it shows that the epiphysis and metaphysis get the good type h vessels but the diaphysis gets the type L vessels. Thus just contracting muscles and building heart rate to increase blood flow will not cut it. You’ll need a stronger force such as lateral impact loading near the metaphysis. To grow taller we’d need a mechanism such as enhanced osteoclast activity degrading cortical bone to allow for interstitial longitudinal bone growth or we’d need fluid movement in the bone directly degrading the cortical bone. Lateral impact should provide the strongest fluid forces needed to stimulate this.
Lateral synovial joint loading should provide some benefit but epiphyseal deformation seems to have a limit and the limit of fluid forces to reach the medullary cavity may be limited by the epiphyseal line.