Me: This is news to me since I haven’t read up on the entire list of 180 genes that affect height in the gene database section. I know that Tyler has talked about LIN28B along with HMGA2. It turns out that the LIB28B gene is actually really influential. It mediates the progenitor cells from bone marrow. Note that the article says that LIN28B is associated with timing of menarche (menarche is the time when a female experiences her first period) so it basically tells the body when to start puberty. From study 2 found below, we can see that in an independent study of over 4,000 women if the major allele of LIN28B is expressed, the menarche occurs earlier by at least 0.1 years, which results in earlier puberty, which leads to eventual less adult height. The ScienceDaily article is based on study 3 found below. The SNP testing of the region around the LIN28B shows it correlated to the timing of growth spurts.
From Science Daily….
Growth Curve Analyses of Finnish Population Shed Light On the Genetic Regulation of Growth in Height
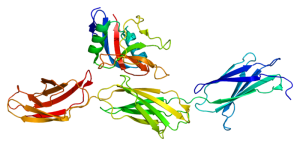
ScienceDaily (Apr. 15, 2010) — Researchers at the University of Helsinki and the Institute for Molecular Medicine Finland (FIMM) have shown that a gene called LIN28B strongly influences height growth from birth to adulthood in a complex and sex-spesific manner.
Human growth in height is a multifaceted process including periods of accelerated and decelerated growth velocities. The postnatal growth trajectory can be conceptualized as consisting of three partially overlapping phases: infant growth characterized by rapidly declining growth velocities, slowly decelerating childhood growth, and the pubertal height growth spurt.
Height is strongly regulated by genes, and so far more than 40 genes have been implicated influencing adult height. Yet, little is known about how individual genes regulate growth in height.
Utilizing the unique resource of longitudinal childhood height growth data available in Finnish population cohorts, researchers at the University of Helsinki and the Institute for Molecular Medicine Finland (FIMM) have pinpointed broad height growth regulating effects to a gene called LIN28B. The same gene is known to be a key regulator of developmental timing in the nematode C. elegans and has previously been associated both with timing of menarche and adult height in humans.
Applying genome-wide association mapping technology, the researchers have now shown that the gene strongly influences the timing of the pubertal height growth spurt both in males and females but they also found that it regulates height growth from birth to adulthood in a complex and sex-specific manner.
“Interestingly; two separate variants of the gene were found to influence growth, one with a more prominent height increasing effect in males and another one increasing height only in females,” tells Academy Research Fellow, Dr. Elisabeth Widén.
Journal Reference:
- Elisabeth Widén , Samuli Ripatti , Diana L. Cousminer , Ida Surakka , Tuuli Lappalainen , Marjo-Riitta Järvelin , Johan G. Eriksson , Olli Raitakari , Veikko Salomaa , Ulla Sovio , Anna-Liisa Hartikainen , Anneli Pouta , Mark I. McCarthy , Clive Osmond , Eero Kajantie , Terho Lehtimäki , Jorma Viikari , Mika Kähönen , Chris Tyler-Smith , Nelson Freimer , Joel N. Hirschhorn , Leena Peltonen and Aarno Palotie.Distinct Variants at LIN28B Influence Growth in Height from Birth to Adulthood. American Journal of Human Genetics, 2010; DOI: 10.1016/j.ajhg.2010.03.010
Nature Genetics 41, 729 – 733 (2009)
Published online: 17 May 2009 | doi:10.1038/ng.382
Genetic variation in LIN28B is associated with the timing of puberty
Ken K Ong1,2,3, Cathy E Elks1,2, Shengxu Li1,2, Jing Hua Zhao1,2, Jian’an Luan1,2, Lars B Andersen4, Sheila A Bingham5,6, Soren Brage1,2, George Davey Smith7, Ulf Ekelund1,2,8, Christopher J Gillson1,2, Beate Glaser7, Jean Golding9, Rebecca Hardy10, Kay-Tee Khaw11, Diana Kuh10, Robert Luben11, Michele Marcus12,13,14, Michael A McGeehin12, Andrew R Ness15, Kate Northstone16, Susan M Ring16, Carol Rubin12, Matthew A Sims1,2, Kijoung Song17, David P Strachan18, Peter Vollenweider19, Gerard Waeber19, Dawn M Waterworth17, Andrew Wong10, Panagiotis Deloukas20, Inês Barroso20, Vincent Mooser17, Ruth J Loos1,2 & Nicholas J Wareham1,2
The timing of puberty is highly variable1. We carried out a genome-wide association study for age at menarche in 4,714 women and report an association in LIN28B on chromosome 6 (rs314276, minor allele frequency (MAF) = 0.33, P = 1.5 × 10−8). In independent replication studies in 16,373 women, each major allele was associated with 0.12 years earlier menarche (95% CI = 0.08–0.16;P = 2.8 × 10−10; combined P = 3.6 × 10−16). This allele was also associated with earlier breast development in girls (P = 0.001; N = 4,271); earlier voice breaking (P = 0.006, N = 1,026) and more advanced pubic hair development in boys (P = 0.01; N = 4,588); a faster tempo of height growth in girls (P = 0.00008; N = 4,271) and boys (P = 0.03; N = 4,588); and shorter adult height in women (P = 3.6 × 10−7; N = 17,274) and men (P = 0.006; N = 9,840) in keeping with earlier growth cessation. These studies identify variation in LIN28B, a potent and specific regulator of microRNA processing2, as the first genetic determinant regulating the timing of human pubertal growth and development.
From PubMed study 2 link HERE…
Am J Hum Genet. 2010 May 14;86(5):773-82. Epub 2010 Apr 15.
Distinct variants at LIN28B influence growth in height from birth to adulthood.
Source
Institute for Molecular Medicine Finland, University of Helsinki, Helsinki, Finland. elisabeth.widen@helsinki.fi
Abstract
We have studied the largely unknown genetic underpinnings of height growth by using a unique resource of longitudinal childhood height data available in Finnish population cohorts. After applying GWAS mapping of potential genes influencing pubertal height growth followed by further characterization of the genetic effects on complete postnatal growth trajectories, we have identified strong association between variants near LIN28B and pubertal growth (rs7759938; female p = 4.0 x 10(-9), male p = 1.5 x 10(-4), combined p = 5.0 x 10(-11), n = 5038). Analysis of growth during early puberty confirmed an effect on the timing of the growth spurt. Correlated SNPs have previously been implicated as influencing both adult stature and age at menarche, the same alleles associating with taller height and later age of menarche in other studies as with later pubertal growth here. Additionally, a partially correlated LIN28B SNP, rs314277, has been associated previously with final height. Testing both rs7759938 and rs314277 (pairwise r(2) = 0.29) for independent effects on postnatal growth in 8903 subjects indicated that the pubertal timing-associated marker rs7759938 affects prepubertal growth in females (p = 7 x 10(-5)) and final height in males (p = 5 x 10(-4)), whereas rs314277 has sex-specific effects on growth (p for interaction = 0.005) that were distinct from those observed at rs7759938. In conclusion, partially correlated variants at LIN28B tag distinctive, complex, and sex-specific height-growth-regulating effects, influencing the entire period of postnatal growth. These findings imply a critical role for LIN28B in the regulation of human growth.
Copyright (c) 2010 The American Society of Human Genetics. Published by Elsevier Inc. All rights reserved.
- PMID: 20398887 [PubMed – indexed for MEDLINE]
- PMCID: PMC2869010