Ever since I found the stories of women who have claimed to have increased in height during pregnancy I decided to do a quick search on google for stories, anecdotal evidence, and posts by women who claim they had gotten taller.
Me: If you read through the comments left by other moms you realize that this phenomena seems to be far more common than I ever expected. Of the 17 replies this women got, a good 2 of them said that they saw an increase in height beyond what would obviously be measurement error. The crazy anedotal story is the man’s wife who grew a “couple” inches when she was 30 and on her 3rd child. Wow, what is going on? Of course it is important to realize that a few of the replies stated that they actually lost height from the pregnancy. I don’t know what to take from this post and the replies except be more confused now.
From this post on an Australian Huggies web board HERE the poster says that she grew 1.5 cm during her pregnancy.
Here is one from CafeMom (source link HERE)
Height growth during pregnancy
I know this may sound weird, but I was talking to someone else today about growing an inch or 2 taller while they were pregnant. I was 5’2″ pre pregnancy and now I’m 5’3 1/2″. This girl is also saying she got taller. I thought it was just the way they measured my height. But can you grow while pregnant?
- Summer222009
on Jul. 6, 2011 at 3:54 AM
- Vipergirl22
Jessica on Jul. 6, 2011 at 5:38 AM
haha I would like to know that answer too…be interesting if it is true.
- KaroGreenly
Karo on Jul. 6, 2011 at 8:30 AM
- .Angelica.
Angie on Jul. 6, 2011 at 9:29 AM
I have heard of this happening. Consider yourself lucky if you wanted to be taller I guess. LOL.
- .Angelica.
Angie on Jul. 6, 2011 at 9:30 AM
A guy my DH works with, when his wife was pregnant with her 3rd child and I think right around 30 she grew a couple inches. So she should have for sure been done growing.
Quoting KaroGreenly:
How old are you? Maybe you just weren’t finished growing to begin with.
- Summer222009
on Jul. 6, 2011 at 2:40 PM
I’m 19 but my growth plates have stopped when I was 12.
Quoting KaroGreenly:
How old are you? Maybe you just weren’t finished growing to begin with.
- momoftwins_2
on Jul. 6, 2011 at 4:34 PM
- ATG499
Wendy on Jul. 6, 2011 at 5:22 PM
- alyciajoseph
on Jul. 6, 2011 at 7:42 PM
Quoting momoftwins_2:
My feet grew but I didn’t get taller
- remaining_me
Kay on Jul. 6, 2011 at 7:55 PM
hmm i never heard of that, lol i didnt get any taller. wider? yes, lol.
- remaining_me
Kay on Jul. 6, 2011 at 7:57 PM
yeah, i permanently went up a half size with my second. I never knew they actually GREW, odd enough. i thought they just swell up.
Quoting momoftwins_2:
My feet grew but I didn’t get taller
11-17 of 17 repliesfirst previous 12 by
by
- Maddies-Mommy
Member on Jul. 7, 2011 at 2:24 AM
I didn’t get taller, however I went up a shoe size. It was weird, they didn’t swell they just got longer and three years later they are still that size. by
by
- lovealot0587
on Jul. 7, 2011 at 2:32 AM
I’m not too surePosted on CafeMom Mobile by
by
- hayvensmommy07
Bronze Member on Jul. 7, 2011 at 9:03 AM
I was 5’2 before my son. Now I’m 5 foot. Yea I shrank. How I have no idea so if I can shrink then I would think women could get taller too.Posted on CafeMom Mobile by
by
- JayBearsmomma
Rachael on Jul. 7, 2011 at 9:47 AM
lol I shrunk and1/2 inch ! I was 5’2 for the longest then at my 6 week check up I was 5’1 1/2Posted on CafeMom Mobile by
by
- YouGotToLoveIt
on Sep. 9, 2011 at 8:11 PM
Hi,
This is my first attempt to investigate my growth during pregnancy on the web. Although I have a friend who grew 1 1/2 inches during her 3rd pregnancy and only daughter.
I am now 60 and had my only child when I was 36. I grew 3/4 of an inch during pregnancy. I tried to document this growth with any of my doctors and they all made excuses saying that they wrote down my original height incorrectly. It was very frustrating because my original height was 5 feet 4 3/4 inches and I always tried to stand super tall when measured so that I could say I was 5 feet 5 inches even. My final height is 5 feet 5 1/2 inches.
Thanks for this forum. It is nice to know that I am not alone.
 by
by
- Girl_Charlie
on Sep. 9, 2011 at 9:39 PM
And you thought that a “young moms” group was the place to go? Even 24 years ago, 36 was on the upper side of having children, not the young side.
Quoting YouGotToLoveIt:
Hi,
This is my first attempt to investigate my growth during pregnancy on the web. Although I have a friend who grew 1 1/2 inches during her 3rd pregnancy and only daughter.
I am now 60 and had my only child when I was 36. I grew 3/4 of an inch during pregnancy. I tried to document this growth with any of my doctors and they all made excuses saying that they wrote down my original height incorrectly. It was very frustrating because my original height was 5 feet 4 3/4 inches and I always tried to stand super tall when measured so that I could say I was 5 feet 5 inches even. My final height is 5 feet 5 1/2 inches.
Thanks for this forum. It is nice to know that I am not alone.
 by
by
- JayBearsmomma
Rachael on Sep. 9, 2011 at 10:28 PM
Lol I shrunk half an inchPosted on CafeMom Mobile
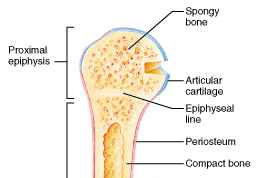
There’s a study that says pregnancy can increase bone turnover. This may be partially the cause of the height gain as bone turnover equals more plastically deformable bones.
The effect of pregnancy on bone density and bone turnover
“We studied 16 women longitudinally, with baseline measurements before pregnancy; then at 16, 26, and 36 weeks of pregnancy; and postpartum. We measured total-body BMD and biochemical markers of bone resorption (urinary pyridinium crosslinks and telopeptides of type I collagen) and bone formation (serum bone alkaline phosphatase, propeptides of type I procollagen [PINP] and osteocalcin). We also measured parathyroid hormone (PTH), insulin-like growth factor I (IGF-I), and human placental lactogen. Postpartum, BMD increased in the arms (2.8%, P < 0.01) and legs (1.9%, P < 0.01) but decreased in the pelvis (-3.2%, P < 0.05) and spine (-4.6%, P < 0.01) compared with prepregnancy values. All biochemical markers, with the exception of osteocalcin concentration, increased during pregnancy. The change in IGF-I at 36 weeks was related to the change in biochemical markers (e.g., PINP, r = 0.72, P = 0.002). Pregnancy is a high-bone-turnover state. IGF-I levels may be an important determinant of bone turnover during pregnancy. Elevated bone turnover may explain trabecular bone loss during pregnancy.”
“The involuting uterus is also a possible source of collagen degradation products. The uterus is predominantly composed of type I collagen; pyridinoline (Pyd) is the principal cross-link, and deoxypyridinoline (Dpd) is present in only trace amounts. The collagen content of the uterus increases approximately sevenfold during pregnancy. An increase in the Pyd/Dpd ratio during the puerperium would indicate a contribution to maternal cross-link excretion from uterine collagen.”
“Previous studies have reported decreased serum intact osteocalcin during pregnancy.”
“there appears to be a loss of bone density at trabecular bone sites and an increase at cortical bone sites during pregnancy. Bone turnover is increased with the increase in bone resorption preceding that of formation.”