1) Stretching(on the spine)
Read this summation of the theory of spinal stretching.
Although one study indicates that a twisting motion can increase height in some cases, other human studies have suggested that twisting can only reduce height in human models. This is due to the nucleus pulposus not being mechanically stable in contrast to the annulus fibrosus which can grow. In response to mechanically strain, there was degeneration in the nucleus pulposus and there is a medical term for this caused degenerative disc disease.
Now, other joints do not have nucleus pulposus like the joints of the ankle and knee so those can potentially grow in size. Interesting though is that one study found that wingspan decreased more with age than overall height. Which is contrary to what we would believe with discs being prone to degeneration. There is an increase in the hand phalanxes continuously throughout life. Now I received an increase of 0.8%(at least) in my right index finger metacarpal. So the normal hand phalanx growth does not explain my growth. That study suggests that articular cartilage can undergo endochondral ossification which can add appositional bone growth to the longitudinal ends of the bone resulting in longitudinal bone growth.
Now one thing is that nucleus pulposus is so prone to degeneration and can reduce height so much is that we can reduce degeneration. For example by living in zero gravity, by strengthening the muscles surrounding the spine to reduce spinal load, or via spinal tractors/inversion to reduce load allowing water to return to the nucleus pulposus.
2) HGH
People have supplemented with HGH at levels at or greater than those who have “suffered” from gigantism reported no height gain. Gigantism does not merely involve elevated HGH levels but also resistance to HGH suppression. Gigantism also involves a tumor. Two factors that are not involved in HGH supplementation.
There has been no evidence as of yet that HGH can induce exogenous growth plates to induce new longitudinal bone growth. Although some anecdotal evidence of HGH induced growth has been reported.
3) Microcracks
There hasn’t been any evidence to suggest that microcracks can lengthen bone. And mineralized bone seems to be incapable of interstitial growth(growth from within ala growth plates) due to high ECM stiffness. Thus there needs to be an intermediary tissue involved like cartilage in order to lengthen bone in a roundabout way. So to lengthen bone via microfractures you’d have to reduce ECM stiffness to allow for interstitial growth. Here’s one possible method to reducing ECM stiffness using acid that has been suggested.
4)Bone Stretching
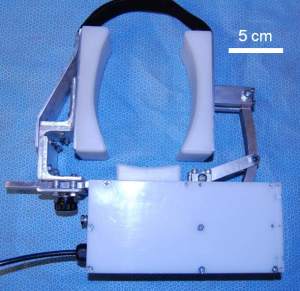
For example via the Rack. The amount of load required to induce a bone fracture is usually a colossal figure like 25000-lbs. And the amount of load to induce plastic deformation(bone stretching or negatively compression) is usually very close to the fracture point. This makes the generation of such loads problematic. That’s why the design of LSJL is to try to induce mesenchymal condensation and neo-growth plate formation.
Creep Strain can induce plastic deformation at much lower loads. However, a considerable continuous amount of load is required to induce 1-2 weeks. I could not find any evidence of creep strain inducing plastic deformation in a positive way(stretching), only a negative way(compression). I couldn’t find any other studies where length was even considered as only damage to the bone was measured.