Development of a Portable Knee Rehabilitation Device That Uses Mechanical Loading
development of portable knee device<-Full study there
“Joint loading is a recently developed mechanical modality, which potentially provides a therapeutic regimen to activate bone formation and prevent degradation of joint tissues. Few joint loading devices are available for clinical or point-of-care applications. Using a voice-coil actuator, we developed an electromechanical loading system appropriate for human studies and preclinical trials that should prove both safe and effective. Two specific tasks for this loading system were development of loading conditions (magnitude and frequency) suitable for humans, and provision of a convenient and portable joint loading apparatus. Desktop devices have been previously designed to evaluate the effects of various loading conditions using small and large animals. However, a portable knee loading device is more desirable from a usability point of view. We present a device that is designed to be portable, providing a compact, user-friendly loader. The portable device was employed to evaluate its capabilities using a human knee model. The portable device was characterized for force-pulse width modulation duty cycle and loading frequency properties. The results demonstrate that the device is capable of producing the necessary magnitude of forces at appropriate frequencies to promote the stimulation of bone growth and which can be used in clinical studies for further evaluations.”
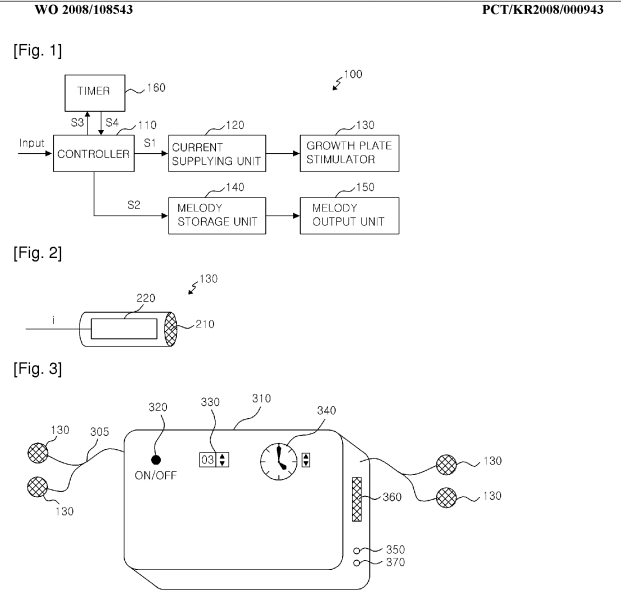
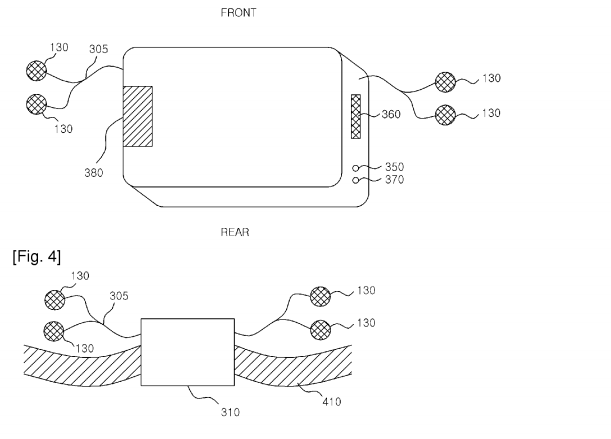
Note how the device looks like a table clamp:


“Dynamic loads applied laterally to the knee joint have been found to stimulate new bone formation not only in the distal femur and proximal tibia epiphyses, but along the entire length of each bone.”
“Knee loading is applied laterally to the epiphysis of the femur and tibia, which consist mostly of trabecular bone modeled to resist axial stresses{if the trabecular bone is modeled to resist axial strain than it is less resistant to lateral strain}. This allows greater deformations than are possible with similar loads in different loading modalities. Dynamic deformations of the epiphysis cause alterations in fluid pressure in the intramedullary cavity, driving oscillatory fluid flow and molecular transport in the lacunocanalicular network in the bone matrix and in the medullary cavity”<-It is alterations in fluid pressure that could induce chondrogenic differentiation of the MSCs in the epiphysis forming new micro growth plates.
“The device applies cyclic loading of magnitudes up to 30N at frequencies ranging from 1 to 20 Hz and can cause small deformation in the knee.”
“The device proposed in this paper differs [from LIPUS and PEMF] in that it stimulates the bone tissue through direct mechanical loading at low frequencies.”
“A cyclic force applied on [the knee] would force a slight shift of the fluid within the bone towards the opposite end of the bone in a controlled fashion.”
“The device must provide sufficient force in a transverse load to the joint without being bulky or unbalanced.”<-This is a problem we may have too. We might have to use a larger clamp for the knee. The standard c-class clamp may work for smaller joints but a larger clamp may perform better for the knee.
“The force magnitudes that the device can produce must be at least 30 N”
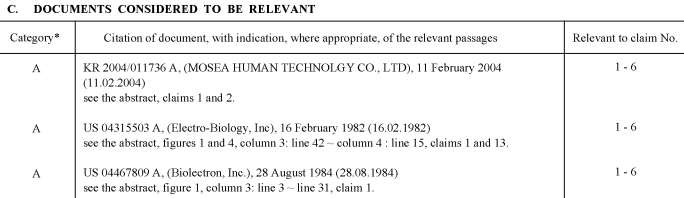
“power generation units used in conjunction with a mechanism comprised of linkages was proposed as a means of shifting the power generation component into a position that allowed for better balance.”
“Operating the device at frequencies between 1 and 5 Hz is meant to simulate the therapeutic and rehabilitative effects of walking or running without the need to put the patient’s weight on the leg.”<-But would the effect be more significant than walking or running? Walking and running have a lot of evidence showing that they don’t make you taller.
“the motor shaft is acting as the sliding block while the linkage connecting to the base plate serves as the crank. The rigid pivot arm that connects the motor shaft and crank before ultimately connecting with the pad at the top is the connecting arm.”<-much like a table clamp.
“Aluminum was chosen for the base plate, side plates, and the adjustable side as it is lightweight, but still provides the necessary strength. The pivot arm and lever arm were made of O1 steel. O1 steel has a high carbon content and a correspondingly high modulus of elasticity. This is crucial as these parts are subjected to higher stresses than are found in any other part of the device; it is important to minimize the deflection in these pieces since deflection of these parts would directly affect the range of displacement provided by the mechanism and may also contribute to damping{a decrease in the amplitude of an oscillation as a result of energy being drained from the system to overcome frictional or other resistive forces.}. High density polyethylene was selected for the pads as it allows a slight amount of deformation to increase comfort to the user while still being sufficiently rigid to transfer most of the force to the knee being loaded.”<-Could be helpful in designing a self-made LSJL device
“For the static loading, a 6.9 kPa pressure is evenly distributed across the 64.5 cm2 surface of both side of the pads directed outwards. A 44.5 N force is applied to the center of the motor shaft pushing away from the motor. This loading simulates the force applied by the motor and the reaction on the pads from the knee being loaded. “<-a lot of studies make it clear though that dynamic load is needed.
According to figure 11, Pressure generated is 6000Pa Or 0.006MPa. Most figures show 0.1 to 10 MPA is what’s needed for chondroinduction but perhaps the pressure generated on the outside is not reflective of the pressure generated inside the bone which could be higher.
Here’s some force generated measurements:

Here’s some displacement measurements:

“the force and corresponding displacement [of the artificial knee] over a period of five cycles at duty cycles of 50% and duty cycles of 100%. Such experiments when performed on an actual knee could be used to assist in the study of the force versus displacement of human tissue, a highly nonlinear reaction, as well as the effects of light mechanical loading to the bone tissue.”
The mechanics definition of displacement is the final position of a point (Rf) relative to its initial position (Ri). Tissue displacement refers to the change in the form or position of the tissues as a result of pressure. So the displacement of the artificial knee was about 2.5mm when the force generated was about 30N. Since the displacement turns to normal it is referred to as an elastic deformation a plastic deformation would be a permanent change. Thus the only way this device can induce new longitudinal bone growth is if it stimulates neo-endochondral ossification.
Here’s some information about the effects of tissue deformation on tissue deformation from a paper called Biomechanics of Tissues from the Journal of Rheumatology: “In a creep test, an instantaneous step or ramp load is applied to the tissue sample and held constant for an extended period of time. This is considered a load control test, and the resulting tissue displacement is measured. The displacement shows an initial elastic response of the tissue followed by a gradual increase of lengthening of the tissue. As the test proceeds, fluid is exuded from the tissue, and the solid components of the tissue are supporting the applied load. A “solid-like” material will be distracted to a point at which the solid components of the tissue will balance the applied load and will not elongate further. The modulus of the tissue is calculated as the stress of the tissue divided by the end displacement of the tissue. A “fluid-like” material will not be able to balance the applied load and will continue to elongate.“<-I don’t believe this occurred during my LSJL finger lengthening as the fingers increased in width greatly as well.
No mention of using the device for lengthening. The basis of using LSJL on lengthening is based on studies that show that hydrostatic pressure can induce chondrogenic differentiation and that LSJL upregulates genes that do not only stimulate chondrogenesis of chondrogenitors but also of MSCs such as FGF-2, Gli3, and Cyr61 and of signs of mesenchymal condensation in LSJL images. Also, in those images is apparent degradation of trabecular bone which would be permissive to neo-growth plate formation.
The condensed stem cells in the images are most consistent with granulocytes which are capable of chondrogenic differentiation. According to Comparative study of the biological characteristics of mesenchymal stem cells from bone marrow and peripheral blood of rats., peripheral blood MSCs are more chondrogenic than bone marrow MSCs but chondrogenesis of bone marrow MSCs is not impossible.
This study does not provide more evidence that LSJL can increase length but it does support the notion that a table clamp is a perfect home made solution for performing LSJL.
Here’s a study with more about the effects of tissue deformation on the joint region:
The effects of manual therapy on connective tissue<-connective tissue therapy
“a low level of CT[connective tissue] damage must occur in order to produce permanent elongation. The collagen breakage will be followed by a classical cycle of tissue inflammation, repair, and remodeling”<-This paper doesn’t mention cartilage specifically but it mentions other tissues made of collagen fibers.
“Connective tissue that is loaded more quickly will behave more stiffly (will deform less) than
the same tissue that is loaded at a slower rate”
In figure 5, a graph is shown where it appears that microfailure of a tissue(the kind of stimulus that must occur in order to generate permanent lengthening of connective tisues) occurs 4-6mm(with a safer region being between 4-4.5mm) of displacement beyond which is complete failure of the tissue. The displacement generated by the LSJL device is 2.5mm which is below this level to generate permanent lengthening of connective tissues.