The reason that the jaw can grow via stretching by forwarding positioning and bite-jumping appliances is that it is not as constrained by ligaments as other bones. It’s possible that other movable joint regions like the wrists, fingers, and toes would also be stretchable. The wrists would come under extreme stress due to the farmers walk so if this true there should be anecdotal evidence of longer arms due to the farmers walk. It is possible that a new height increase method could be invented that causes enough tensile strain in the articular cartilage to activate endochondral ossification in that region. The ligaments holding the bone together would constrain this. This would also help explain why people with Marfan’s become taller as they have more flexible joints and therefore their growth is less constrained by ligaments. Here’s another connective tissue disorder that may affect longitudinal bone growth. It’s also possible that differences between condylar cartilage and articular cartilage allow this to happen in the mandible but not in other joints.
So if anyone could look for instances of longer arms due to heavy farmers walk. This would be much easier to do than LSJL. So any research on this would be a great boon to further the cause of height increase.
The adaptive remodeling of condylar cartilage—a transition from chondrogenesis to osteogenesis.
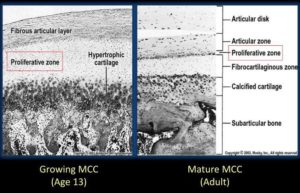
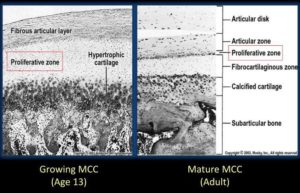
“Mandibular condylar cartilage is categorized as articular cartilage but markedly distinguishes itself in many biological aspects, such as its embryonic origin, ontogenetic development, post-natal growth mode, and histological structures. The most marked uniqueness of condylar cartilage lies in its capability of adaptive remodeling in response to external stimuli during or after natural growth. The adaptation of condylar cartilage to mandibular forward positioning{basically bringing your jaw forward} constitutes the fundamental rationale for orthodontic functional therapy, which partially contributes to the correction of jaw discrepancies by achieving mandibular growth modification. The adaptive remodeling of condylar cartilage proceeds with the biomolecular pathway initiating from chondrogenesis and finalizing with osteogenesis{so basically by stretching the articular cartilage you activate enchondral ossification enabling you to grow on the longitudinal ends of the bone}. During condylar adaptation, chondrogenesis is activated when the external stimuli, e.g., condylar repositioning, generate the differentiation of mesenchymal cells in the articular layer of cartilage into chondrocytes, which proliferate and then progressively mature into hypertrophic cells. The expression of regulatory growth factors, which govern and control phenotypic conversions of chondrocytes during chondrogenesis, increases during adaptive remodeling to enhance the transition from chondrogenesis into osteogenesis, a process in which hypertrophic chondrocytes and matrices degrade and are replaced by bone. The transition is also sustained by increased neovascularization, which brings in osteoblasts that finally result in new bone formation beneath the degraded cartilage. The repositioning of the mandibular condyle in adult rats led to a reactivation of chondrogenesis in condylar cartilage which otherwise is at resting status, and finally results in increased bone formation{this is huge if as it means a bigger stronger jaw}”
“chondrogenic activity of BMP-2 in vitro involves the action of the cell-cell adhesion protein, N-cadherin, which functionally complexes with beta-catenin the change of condyle position relative to the glenoid fossa constitutes an important trigger for [the endochondral ossification related adaptation of the mandible].”
The deviation of the condyle from the glenoid fossa by mandibular forward translation is the basis for orthodontic functional therapy, which aims to enhance condylar growth and therefore to eliminate the discrepancy between upper and lower jaws.
“a decrease in compressive loading enhances condylar growth, whereas an increase in loading inhibits growth”
Note that they do say that condylar cartilage is distinct from articular cartilage.
Here’s another study:
Murine TMJ loading causes increased proliferation and chondrocyte maturation.
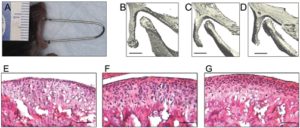
“The purpose of this study was to examine the effects of forced mouth opening on murine mandibular condylar head remodeling. We hypothesized that forced mouth opening would cause an anabolic response in the mandibular condylar cartilage. Six-week-old female C57BL/6 mice were divided into 3 groups: (1) control, (2) 0.25 N, and (3) 0.50 N of forced mouth opening. Gene expression, micro-CT, and proliferation were analyzed. 0.5 N of forced mouth opening caused a significant increase in mRNA expression of Pthrp, Sox9, and Collagen2a1, a significant increase in proliferation{These alone will not increase height except maybe the increase in proliferation}, and a significant increase in trabecular spacing in the subchondral bone, whereas 0.25 N of forced mouth opening did not cause any significant changes in any of the parameters examined. Forced mouth opening causes an increase in the expression of chondrocyte maturation markers and an increase in subchondral trabecular spacing.”
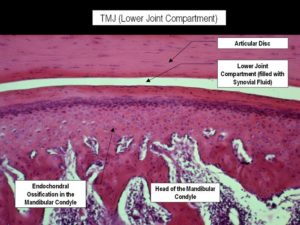
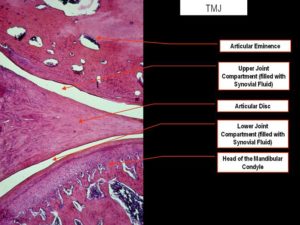
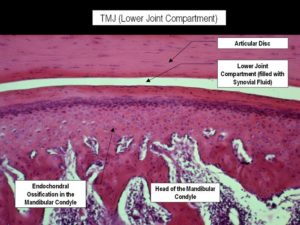
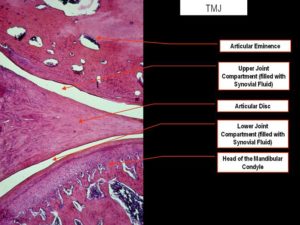
“The articulating surfaces of the temporomandibular joint (TMJ) are covered by fibrocartilage, which is composed of chondrocytes at various stages of maturation that are organized into four zones: (1) superior articular zone—cells in this zone express proteoglycan 4 (Prg4); (2) polymorphic zone—cells in this zone express SRY-box 9 (Sox9) and parathyroid-hormone-related protein (Pthrp); (3) flattened zone—the cartilage cells in this layer express collagen type II (Col 2a1); and (4) hypertrophic zone—the chondrocytes express collagen type X (Col 10a1)”
“Growth in the condylar cartilage proceeds from cells exiting the proliferative pool in the polymorphic zone and undergoing endochondral ossification in the inferior cartilage zones. The mandibular condylar cartilage is able to remodel its structure in response to mechanical strains”

F and G are both forced mouth opening with F and G to a higher degree. C and D have longer bones but there is less separation between the two bones with C and D. The fear with articular cartilage endochondral ossification is that you’ll decrease the joint space.
“Functional appliance therapy is believed to place the mandible in a protrusive position, causing the condyle to be unseated caudally and ventrally from the articular fossa, while forced mouth opening is believed to cause a compressive force between the articular eminence and the mandibular condyle”
“A possible explanation for both functional appliance therapy and forced mouth opening causing similar effects in the mandibular condylar cartilage is that the mandibular condylar cartilage responds similarly to different types of loading compression for forced mouth opening and tension for functional appliance therapy{another possibility is that both activate the lateral pterygoid muscle and that’s what pulls on the cartilage}. Another possible explanation is that forced mouth opening and functional appliance therapy influence the masticatory muscles in such a way that the actual deformational strains within the mandibular condylar cartilage are similar for both.”
Forward mandibular positioning enhances the expression of Ang-1 and Ang-2 in rabbit condylar chondrocytes
“Functional appliances correct dental malocclusion, partly by exerting an indirect mechanical stimulus on the condylar cartilage, initiating novel bone formation in the condyle. Angiopoietin is involved in the angiogenesis associated with novel bone formation. This study aimed to determine the expression of angiopoietin (Ang)‑1 and ‑2 following forward mandibular positioning (FMP) in the condylar chondrocytes of rabbits. Sixty rabbits (age, 8 weeks) were randomly allocated to the experimental and control groups (n=30 per group). In the experimental group, FMP was induced by a functional appliance. Five rabbits from the experimental group and the control group were sacrificed following 3 days and 1, 2, 4, 8 and 12 weeks, respectively. The right temporomandibular joints (TMJs) were collected and the expression of Ang‑1 and -2 was evaluated by immunohistochemical staining. The expression of Ang-1 increased at day 3 and reached a peak at 2 weeks, whereas Ang‑2 reached maximal expression 4 weeks after FMP. Subsequently, the expression of Ang‑1 and ‑2 gradually decreased. Thus, FMP enhanced the expression of Ang‑1 and Ang‑2 in condylar cartilage, which is related to angiogenesis in the process of endochondral ossification.”
“Autocrine Ang-1/Tie-2 modulates blood vessel plasticity and contributes to vascular maintenance. In addition, Ang-1 enhances survival, migration and network formation of endothelial cells in vitro, and induces neovascularization in vivo. Ang-2 is a naturally occurring antagonist of Ang-1 that inhibits Ang-1-induced activation of Tie2. Ang-1 and -2 are located at sites of endochondral bone formation in the growing skeleton”
“The appliances were worn for 24 h to produce a continuous forward and downward positioning of the mandible.”

Look at all the cartilage growth. There seems to be some endochondral ossification going on in the longitudinal ends of bone which is very good for height growth.
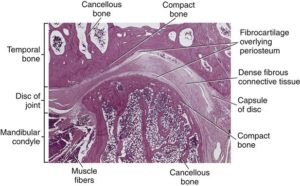
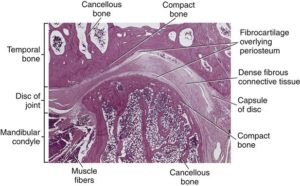
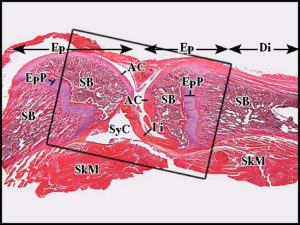
Here’s a normal joint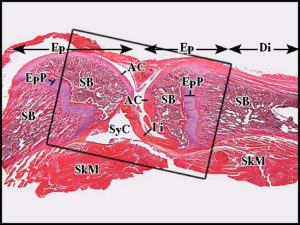 Notice how they are connected strongly by a ligament(Li)
Notice how they are connected strongly by a ligament(Li)
Here’s Mandibular Condylar Cartilage as a Juvenile and as an adult: